Overview
Female urinary system
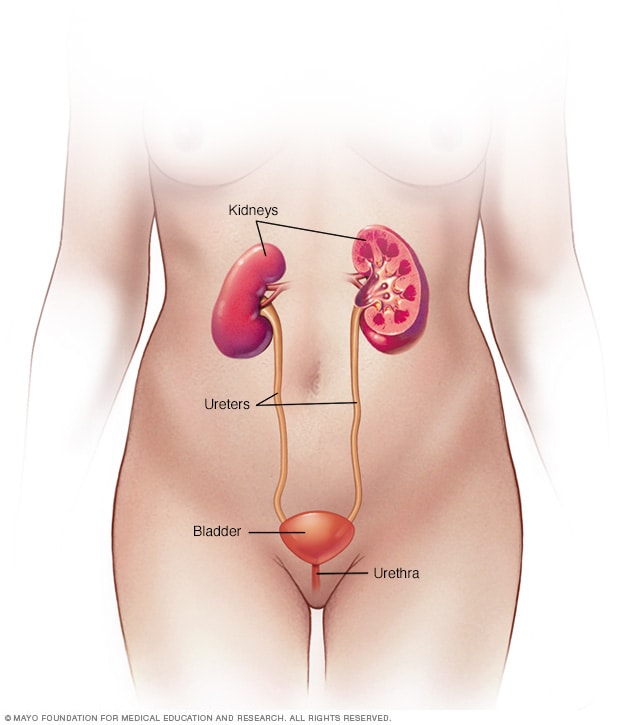
Female urinary system
The urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys sit toward the back of the upper abdomen. They filter waste and fluid from the blood and make urine. Urine moves from the kidneys to the bladder through narrow tubes called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through a small tube called the urethra.
Male urinary system
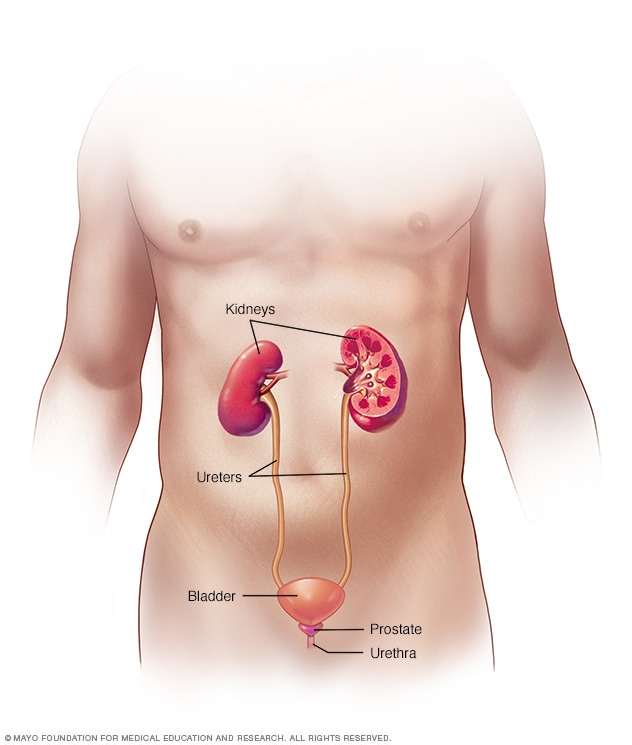
Male urinary system
The urinary system includes the kidneys, ureters, bladder and urethra. The urinary system removes waste from the body through urine. The kidneys sit toward the back of the upper abdomen. They filter waste and fluid from the blood and make urine. Urine moves from the kidneys through narrow tubes to the bladder. These tubes are called the ureters. The bladder stores urine until it's time to urinate. Urine leaves the body through a small tube called the urethra.
Urinary incontinence is the loss of bladder control. Stress incontinence happens when movement or activity puts pressure on the bladder, causing urine to leak. Movements include coughing, laughing, sneezing, running or heavy lifting. Stress incontinence is not related to mental stress.
Stress incontinence is not the same as urgency incontinence and overactive bladder (OAB). Those conditions cause the bladder muscle to spasm. This leads to a sudden need to urinate quickly. Stress incontinence is much more common in women than in men.
If you have stress incontinence, you may feel ashamed. You might limit your work and social life because you don't want to be with others. You also might not do physical or fun activities.
Treatment can help you manage stress incontinence and improve your quality of life.
Products & Services
Symptoms
If you have stress incontinence, you may leak urine when you:
- Cough or sneeze.
- Laugh.
- Bend over.
- Lift something heavy.
- Exercise.
- Have sex.
You might not leak urine every time you do one of these things. But any activity that puts pressure on your bladder can make leaking more likely. Having a full bladder increases the chances of leaking.
When to see a doctor
Talk to your healthcare professional if your symptoms bother you or get in the way of daily activities like work, hobbies and social life.
Causes
Female pelvic floor muscles
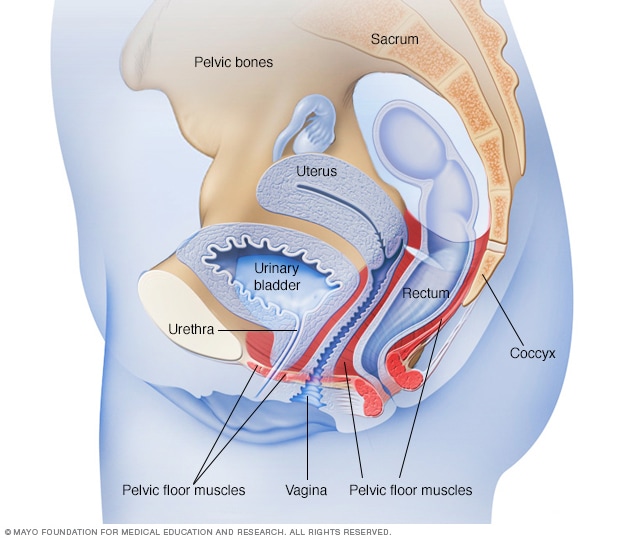
Female pelvic floor muscles
The pelvic floor muscles support the pelvic organs. Those organs include the uterus, bladder and rectum. Kegel exercises can help strengthen the pelvic floor muscles.
Male pelvic floor muscles
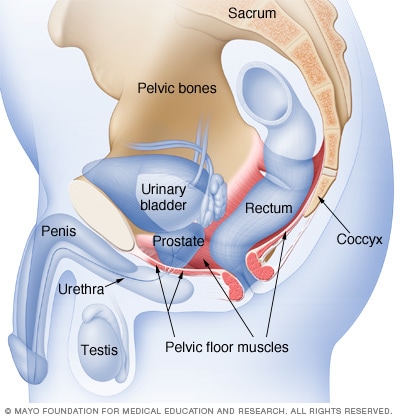
Male pelvic floor muscles
The male pelvic floor muscles support the bladder and bowel and affect sexual function. Kegel exercises can help strengthen these muscles.
Stress incontinence happens when certain muscles and other tissues linked to urinating weaken. These include the muscles that support the urethra, called the pelvic floor muscles, and the muscles that control the release of urine, called the urinary sphincter.
The bladder expands as it fills with urine. Most often, valve-like muscles in the tube that carries urine out of the body, called the urethra, stay closed as the bladder expands. This keeps you from leaking urine until you reach a bathroom.
But when those muscles weaken, anything that puts force on the stomach and pelvic muscles put pressure on your bladder. Sneezing, bending over, lifting or laughing hard, for instance, can cause urine leakage.
Female stress incontinence
In people assigned female at birth, the pelvic floor muscles and urinary sphincter may lose strength because of:
- Childbirth. Tissue or nerve damage during delivery of a child can weaken the pelvic floor muscles or the sphincter. Stress incontinence from this damage may begin soon after delivery or happen years later.
Male stress incontinence
In people assigned male at birth, the pelvic floor muscles and urinary sphincter may lose strength because of:
- Prostate surgery. Treatment for prostate cancer often involves surgery to remove the prostate gland, called a prostatectomy. This surgery is the most common factor leading to stress incontinence. This procedure can weaken the sphincter, which lies right below the prostate gland and goes around the urethra.
Other factors
Other factors that can make stress incontinence worse for males and females include:
- Illnesses that cause chronic coughing.
- Obesity.
Risk factors
Factors that increase the risk of getting stress incontinence include:
- Age. Physical changes that happen with age, such as muscles getting weaker, may make you more likely to get stress incontinence. But some stress incontinence can happen at any age.
- Body weight. People who are overweight or obese have a higher risk of stress incontinence. Excess weight increases pressure on the abdominal and pelvic organs.
For females, risks factors also include:
- Type of childbirth delivery. People who've had a vaginal delivery are more likely to have urinary incontinence than are those who had a cesarean section. Having more than one child also raises the risk.
Complications
Complications of stress incontinence may include:
- Emotional upset. If you have stress incontinence, you may feel embarrassed. It can disrupt your work, social life, relationships and even your sex life. Some people are ashamed that they need pads or incontinence garments.
- Mixed urinary incontinence. It's common to have both stress incontinence and urgency incontinence. Urinary incontinence results when bladder muscles tighten and cause an urgent need to urinate. People with this condition may have frequent urination, urination in the evening and urgency to urinate with or without associated incontinence. This is called overactive bladder.
- Skin rash or soreness. Prolonged contact with urine can cause skin to be sore or to break down. This can happen with severe incontinence if you don't use moisture barriers or incontinence pads. Change pads often and use continence pads rather than menstrual pads to prevent skin sores.
Feb. 14, 2024