Diagnosis
Your healthcare professional may ask about your symptoms and medical history. You may have a physical exam. You also may need an imaging test to help find the problem.
Imaging tests
These tests may include:
- X-rays. An X-ray of the back can show bone changes that may be making the space within the spinal canal smaller. Each X-ray involves a small dose of radiation.
- Magnetic resonance imaging (MRI). An MRI uses a powerful magnet and radio waves to produce detailed images of hard and soft tissue. The test can detect damage to the disks and ligaments. It also can show whether tumors are present.
- Computerized tomography (CT). If you can't have an MRI, you may need a CT scan. This test combines X-ray images taken from many different angles. In a CT myelogram, a contrast dye is injected to outline the spinal cord and nerves. This can show herniated disks, bone spurs and tumors.
More Information
Treatment
Treatment for spinal stenosis depends on how severe your symptoms are.
Medicines
Your healthcare professional might prescribe:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). If common pain relievers don't provide enough relief, prescription NSAIDs might be helpful.
- Antidepressants. Nightly doses of tricyclic antidepressants, such as amitriptyline, can help ease chronic pain.
- Anti-seizure drugs. Some anti-seizure drugs, such as gabapentin (Neurontin, Gralise), are used to reduce pain caused by damaged nerves.
- Opioids. Medications such as oxycodone (Oxycontin, Roxicodone, others) may be used but can be habit-forming.
Physical therapy
A physical therapist can teach you exercises that may help:
- Build up your strength and endurance.
- Maintain the flexibility and stability of your spine.
- Improve your balance.
Steroid shots
Your nerve roots may become irritated and swollen at the spots where they are being pinched. Injecting a steroid medicine into the space around the pinched nerve may help reduce the swelling and relieve some of the pain.
However, steroid shots may not be the best choice for spinal stenosis. Some studies have shown that combined injections of steroids and a numbing medicine relieve back pain no better than shots of numbing medicine alone.
This is important because steroids can cause serious side effects. Repeated steroid injections can weaken nearby bones, tendons and ligaments. That's why a person often must wait many months before getting another steroid injection.
Needle procedure for thickened ligaments
Sometimes, the ligament at the back of the lower spine, also called the lumbar spine, gets too thick. Needlelike tools inserted through the skin can remove some of the ligament. This can create more space in the spinal canal to reduce pressure on nerve roots. You may be given medicine to help you feel calm during the procedure. Many people can go home the same day.
Surgery
Laminectomy
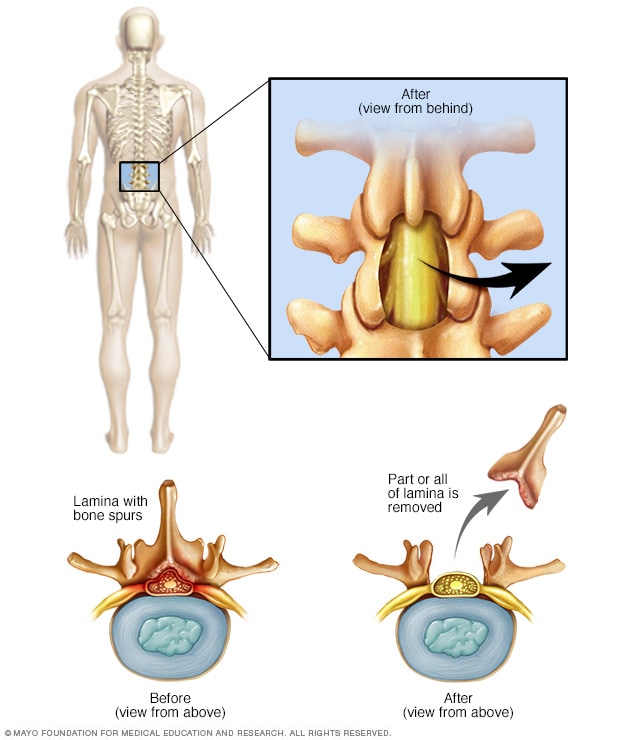
Laminectomy
A lumbar laminectomy involves the removal of the back part of a vertebra in your lower back to make more room within the spinal canal.
Cervical laminectomy
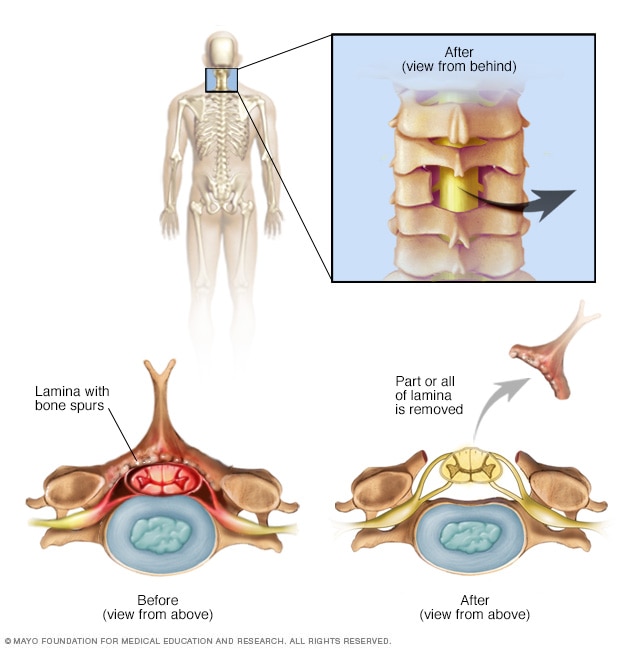
Cervical laminectomy
A cervical laminectomy involves the removal of the back part of a vertebra in your neck to make more room within the spinal canal.
Laminotomy
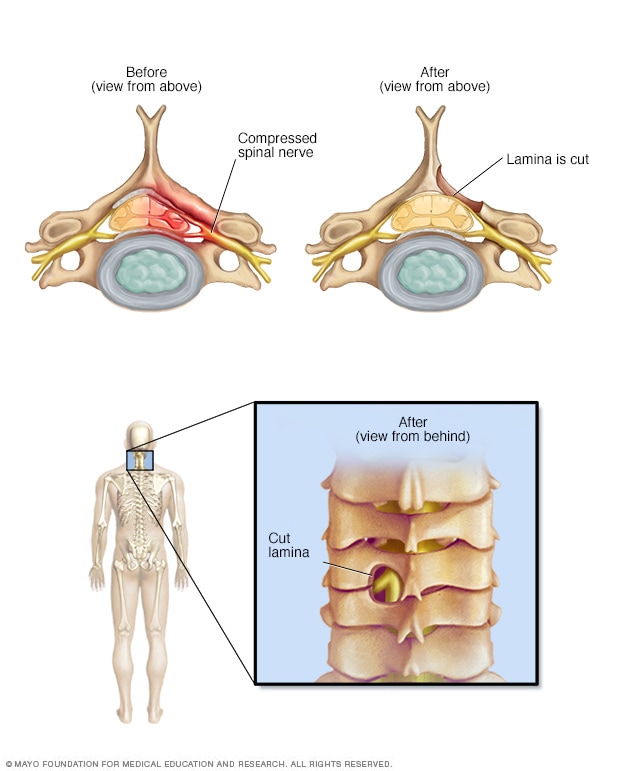
Laminotomy
A laminotomy removes only a portion of the lamina, the back part of a spinal bone. It carves a hole just big enough to relieve the pressure in a specific spot. While shown here on the neck, the surgery also can be done in the lumbar spine.
Laminoplasty
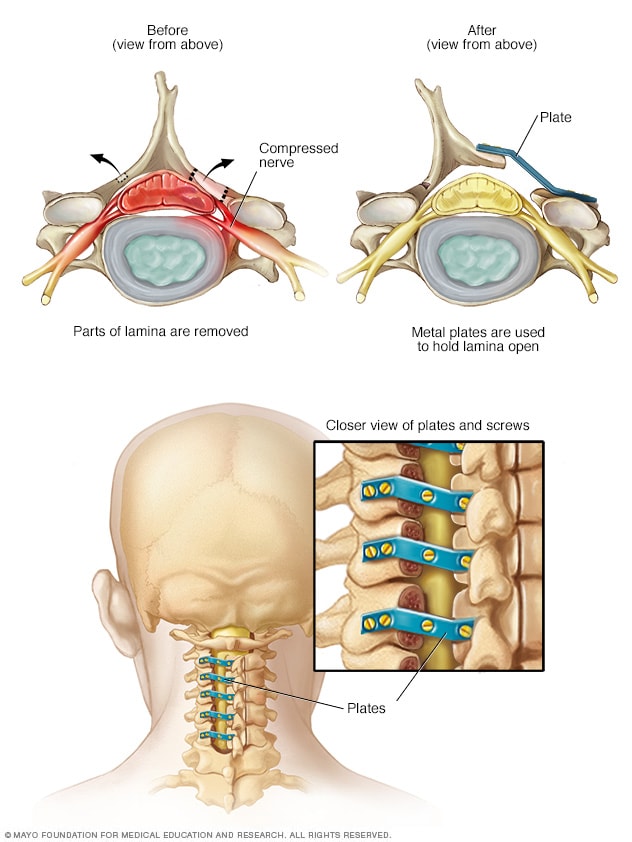
Laminoplasty
Laminoplasty is done only on the spinal bones in the neck. It increases the space within the spinal canal by creating a hinge on the lamina, the back part of a spinal bone. Metal hardware bridges the gap in the opened section of the spine.
Surgeries to create more space within the spinal canal may include:
- Laminectomy. This surgery removes the back part of the affected spinal bone. This part of the bone is called the lamina. This process eases pressure on the nerves by making more space around them. Sometimes, that bone may need to be linked to nearby spinal bones with metal hardware and a bone graft.
- Laminotomy. This surgery removes only part of the lamina. The surgeon carves a hole just big enough to relieve pressure in a specific spot.
- Laminoplasty. This surgery is done only on spinal bones in the neck. It makes the space within the spinal canal bigger by creating a hinge on the lamina. Metal hardware bridges the gap in the opened section of the spine.
In most cases, these operations help reduce spinal stenosis symptoms. But some people's symptoms stay the same or get worse after surgery. Surgical risks include:
- Infection.
- Blood clot in a leg vein.
- Tear in the membrane that covers the spinal cord.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Your healthcare professional may suggest:
- Pain relievers. Medicines you can buy without a prescription — such as aspirin, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and acetaminophen (Tylenol, others) — can help reduce pain and swelling.
- Weight loss. Losing excess weight can reduce pain by taking some stress off the lower back.
- Exercise. Stretching and strengthening exercises may help relieve symptoms. Talk with your healthcare team about what exercises are safe to do at home.
- Walking aids. In addition to providing stability, canes and walkers can help relieve pain by allowing you to bend forward while walking.
Alternative medicine
Integrative medicine and alternative therapies may be used with conventional treatments to help you cope with spinal stenosis pain. Examples include:
- Massage therapy.
- Chiropractic treatment.
- Acupuncture.
Preparing for your appointment
You might be referred to a doctor who specializes in disorders of the nervous system, called a neurologist. Depending on how serious your symptoms are, you also may need to see a spinal surgeon, which could be a neurosurgeon or an orthopedic surgeon.
What you can do
Before the appointment, you might want to prepare a list of answers to the following questions:
- When did you first notice this problem?
- Has it worsened with time?
- Have your parents or siblings ever had similar symptoms?
- Do you have other medical problems?
- What medicines or supplements do you take regularly?
- What spine surgeries or injections have you had?
What to expect from your doctor
Your healthcare professional may ask some of the following questions:
- Do you have pain? Where is it?
- Does any position ease the pain or worsen it?
- Do you have any weakness, numbness or tingling?
- Do you feel clumsier lately?
- Have you had any difficulty controlling your bowel or bladder?
- What treatments have you tried already for these problems?