Diagnosis
To find out what kind of scrotal mass you have, you may need tests such as:
- A physical exam. During this exam, a doctor or other health care professional feels your scrotum, its contents and nearby areas of the groin while you stand and lie down.
- Transillumination. Shining a bright light through the scrotum might provide information about the size, location and makeup of a scrotal mass.
- Ultrasound. This test uses sound waves to make an image of the inside of the body. It can provide detailed information about the size, location and makeup of a scrotal mass. It also can show the condition of the testicles. An ultrasound often is needed to diagnose a scrotal mass.
- Urine test. Lab tests of a sample of urine might find an infection caused by a virus or bacteria. A urine test also might detect the presence of blood or pus in the urine.
- Blood test. Lab tests of a blood sample might find a bacterial or viral infection. Or they might detect higher levels of certain proteins that are linked with testicular cancer.
- Computerized tomography (CT) scan. If other tests show you have testicular cancer, you'll likely get this series of X-rays. A CT scan of your chest, stomach area and groin can check to see if cancer has spread to other tissues or organs.
Treatment
Treatment of a scrotal mass mainly depends on its cause.
Infections
Medicines called antibiotics can treat a scrotal mass caused by bacteria, as is often the case with epididymitis. If a virus causes epididymitis or orchitis, the usual treatment involves rest, ice and pain relief medicine.
Scrotal masses that aren't cancer
You might hear these called benign masses. Sometimes they don't need treatment. Other times, they need to be removed with surgery, repaired or drained. Treatment decisions depend on factors such as whether the scrotal mass:
- Causes discomfort or pain.
- Contributes to or raises the risk of infertility.
- Becomes infected.
Testicular cancer
If your scrotal mass is caused by cancer that starts in a testicle, you'll likely see a cancer doctor called an oncologist. The oncologist may recommend treatments based on whether the cancer is in the testicle or has spread to other body parts. Your age and overall health also are factors.
The main treatment choices include:
- Radical inguinal orchiectomy. This is the main treatment for testicular cancer. It's surgery to remove the affected testicle and the spermatic cord through a cut in the groin. Lymph nodes in your stomach area also might be removed if the cancer has spread to them.
- Chemotherapy. This uses powerful chemicals to kill cancer cells. Most often, you receive chemo through a needle in a vein. It's often used to cure testicular cancer that has spread beyond the testicle. It also is used to lower the chances of the cancer coming back after a testicle is removed with surgery. Chemo isn't a treatment for cancer that's only in the testicle.
Radiation therapy also may be used. It sends high-dose X-rays or other high-energy radiation to specific parts of the body. This can kill cancer cells or slow them from growing. With testicular cancer, the main use for radiation is to destroy cancer cells that have spread to the lymph nodes. Your provider may recommend this treatment after surgery to remove an affected testicle.
Most cases of early testicular cancer can be cured. And even if the disease spreads beyond the testicle, it still may be curable. But you'll need follow-up care to watch for signs that the cancer has come back.
Lifestyle and home remedies
Testicular self-exam
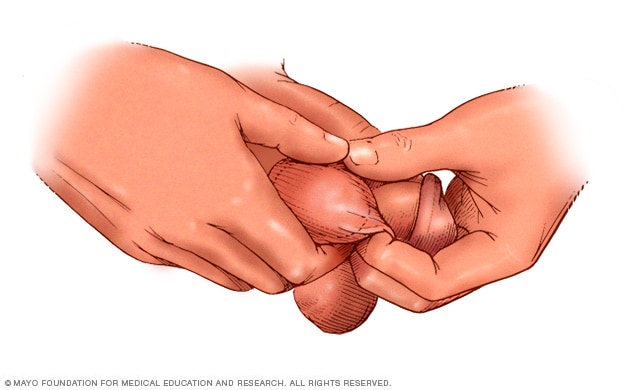
Testicular self-exam
To perform a testicular self-exam, grasp and roll the testicle between your thumbs and forefingers, feeling for lumps, swelling, hardness or other changes.
Self-exams of the testicles might help you find a scrotal mass early on. To do a self-exam, follow these steps:
- Check your testicles once a month. This is key if you've had testicular cancer or if a blood relative, such as your father or brother, has had it.
- Do the exam after a warm bath or shower. The heat from the water relaxes your scrotum, making it easier for you to check.
- Stand in front of a mirror. Look for swelling on the skin of the scrotum.
- Cup your scrotum with one hand to see if it feels different than usual.
- Check one testicle at a time using both hands. Place the index and middle fingers under the testicle; place your thumbs on top.
- Gently roll the testicle between the thumbs and fingers to feel for lumps. The testicles are usually smooth, oval shaped and somewhat firm. Often, one testicle is slightly larger than the other.
- Feel along the soft, comma-shaped structure that runs above and behind the testicle, called the epididymis, to check for swelling.
If you find a lump or other unusual change, seek medical care to get it checked as soon as you can.
Preparing for your appointment
Get emergency care if you have pain in your scrotum or testicles. If you find a scrotal mass, you'll probably start by seeing your doctor or other health care professional. You might be referred to a doctor called a urologist, who treats urinary tract and male genital conditions.
Preparing for the appointment helps you make the most of your time during the visit.
What you can do
Write down information to share with your care team, such as:
- Your symptoms, including any that may seem unrelated to a scrotal mass.
- Key personal information, including major stresses or recent life changes.
- Medicines, vitamins and supplements you take.
- Family history of testicular cancer or other health problems with the scrotum.
- Personal medical history, including previous scrotal masses, undescended testicle or genital conditions you were born with.
- Questions to ask your care team.
Questions you could ask about scrotal masses include:
- What tests will I need?
- How long will it take to get the test results?
- If the scrotal mass is cancerous, what are the next steps?
- If the scrotal mass isn't cancerous, will I need treatment?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
Don't hesitate to ask any other questions.
What to expect from your doctor
Be prepared to answer many questions, including:
- When did you find a lump or notice other symptoms linked with a scrotal mass?
- Do you have pain in or near your scrotum?
- Have you had a fever or seen blood or pus in your urine?
- Have you had a recent injury to the groin?
- Does anything, such as pain medicine, make your symptoms better? Does anything make your symptoms worse, such as exercise or activities that put a strain on the groin?
- Did you have an undescended testicle that was corrected with surgery?
- Have you ever had a sexually transmitted infection? Do you have more than one sex partner or a new sex partner?
Aug. 04, 2023