Overview
Pulmonary hypertension
Pulmonary hypertension
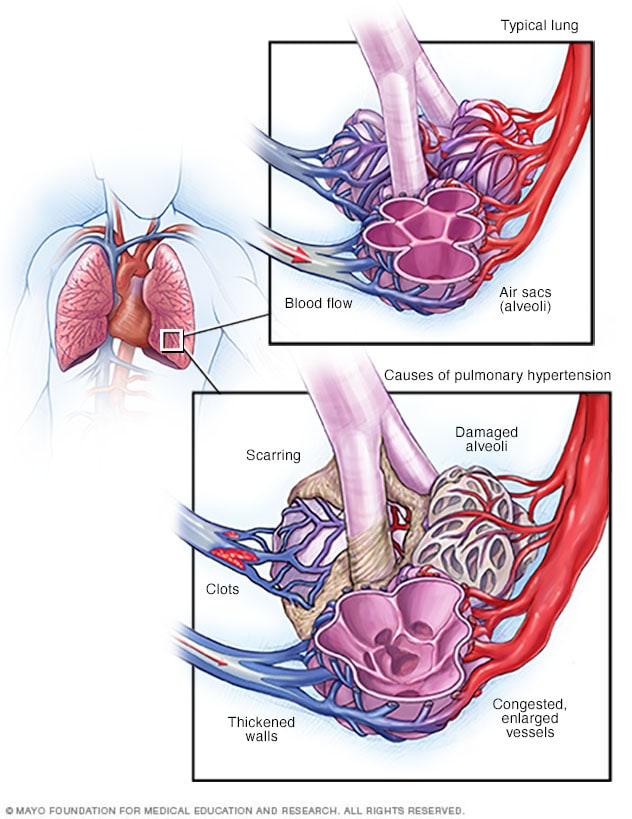
When blood vessels in the lungs become thickened, narrowed, blocked or destroyed, it's harder for blood to flow through the lungs. As a result, blood pressure goes up in the lungs. This condition is called pulmonary hypertension.
Pulmonary hypertension is a type of high blood pressure that affects the arteries in the lungs and the right side of the heart.
In one form of pulmonary hypertension, called pulmonary arterial hypertension (PAH), blood vessels in the lungs are narrowed, blocked or destroyed. The damage makes it hard for blood to move through the lungs. Blood pressure in the lung arteries goes up. The heart must work harder to pump blood through the lungs. The extra effort eventually causes the heart muscle to become weak and fail.
In some people, pulmonary hypertension slowly gets worse. It can be life-threatening. There's no cure for pulmonary hypertension. But treatments are available to help you feel better, live longer and improve your quality of life.
Products & Services
Symptoms
The symptoms of pulmonary hypertension develop slowly. You may not notice them for months or even years. Symptoms get worse as the disease continues.
Pulmonary hypertension symptoms include:
- Shortness of breath. It may first start during exercise and eventually happen at rest.
- Blue or gray skin. Depending on skin color, these changes may be harder or easier to see.
- Chest pressure or pain.
- Dizziness or fainting.
- Fast pulse or pounding heartbeat.
- Fatigue.
- Swelling in the ankles, legs and belly area.
These symptoms may be caused by many other health conditions. See a healthcare professional for an accurate diagnosis.
Causes
Pulmonary hypertension is caused by changes in the cells that line the lung arteries. The changes can make the artery walls narrow, stiff, swollen and thick. It gets harder for blood to flow through the lungs.
Pulmonary hypertension is sorted into five groups, depending on the cause.
Group 1: Pulmonary arterial hypertension (PAH)
Causes include:
- Unknown cause, called idiopathic pulmonary arterial hypertension.
- Changes in a gene passed down through families, called heritable pulmonary arterial hypertension.
- Use of some medicines or illicit drugs, including methamphetamine.
- Heart condition present at birth, called a congenital heart defect.
- Other health conditions, including scleroderma, lupus and cirrhosis.
Group 2: Pulmonary hypertension caused by left-sided heart disease
This is the most common form of pulmonary hypertension. Causes include:
- Left heart failure.
- Left-sided heart valve disease, including mitral valve or aortic valve disease.
Group 3: Pulmonary hypertension caused by lung disease
Causes include:
- Scarring of the lungs, called pulmonary fibrosis.
- Chronic obstructive pulmonary disease, also called COPD.
- A sleep disorder in which breathing repeatedly stops and starts, called sleep apnea.
- Being at high altitudes for extended periods of time, if you are at high risk of pulmonary hypertension.
Group 4: Pulmonary hypertension caused by blockages in the pulmonary artery
Causes include:
- Blood clots in the lungs that don't go away.
- Tumors that block the pulmonary artery.
Group 5: Pulmonary hypertension triggered by other health conditions
Causes include:
- Blood disorders, including polycythemia vera and essential thrombocythemia.
- Inflammatory disorders such as sarcoidosis.
- Conditions that affect the body's ability to break down certain sugars, including glycogen storage disease.
- Kidney disease.
Eisenmenger syndrome and pulmonary hypertension
Eisenmenger syndrome can lead to pulmonary hypertension.
Eisenmenger syndrome is a long-term complication of an unrepaired heart condition present at birth. An example is a large hole in the heart between the two lower heart chambers called a ventricular septal defect.
The unrepaired hole in the heart causes oxygen-rich blood to mix with oxygen-poor blood. The blood then goes to the lungs instead of going to the rest of the body. This increases pressure in the pulmonary arteries.
Risk factors
Pulmonary hypertension is usually seen in people ages 30 to 60. Growing older can increase the risk of developing Group 1 pulmonary hypertension, called pulmonary arterial hypertension (PAH). PAH from an unknown cause is more common in younger adults.
Other things that can raise the risk of pulmonary hypertension are:
- A family history of the condition.
- Being overweight.
- Smoking.
- Blood-clotting disorders or a family history of blood clots in the lungs.
- A history of being around asbestos.
- A heart condition present at birth, called a congenital heart defect.
- Living at an altitude of 8,000 feet (2,438 meters) or higher.
- Use of some medicines, including those used for weight loss.
- Illicit drugs such as cocaine or methamphetamine.
Complications
Potential complications of pulmonary hypertension are:
-
Right-sided heart enlargement and heart failure. Also called cor pulmonale, this condition causes the heart's right lower chamber to get larger. The chamber has to pump harder than usual to move blood through narrowed or blocked lung arteries.
As a result, the heart walls get thick. The right lower heart chamber stretches to increase the amount of blood it can hold. These changes create more strain on the heart. Eventually the right lower heart chamber fails.
- Blood clots. Pulmonary hypertension increases the risk of blood clots in the small arteries in the lungs.
- Irregular heartbeats, also called arrhythmias. Pulmonary hypertension can cause changes in the heartbeat, which can be life-threatening.
- Bleeding in the lungs. Pulmonary hypertension can lead to life-threatening bleeding in the lungs and coughing up blood.
- Pregnancy complications. Pulmonary hypertension can be life-threatening for the mother and the developing baby.