Overview
Bile duct damage
Bile duct damage
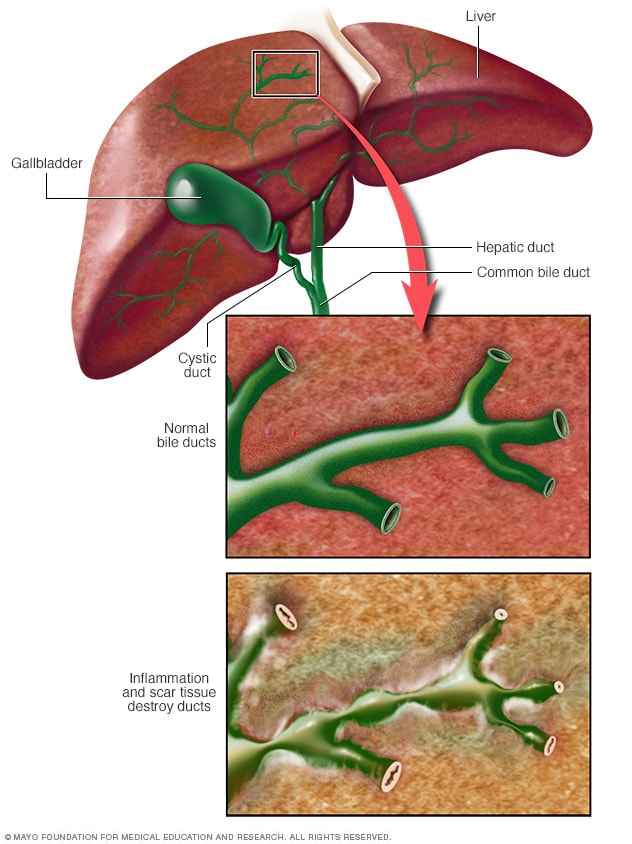
Bile ducts carry bile from the liver to the small intestine. Bile helps break down fats. When bile ducts become damaged, bile can back up into the liver, causing damage to liver cells. This damage can lead to liver failure.
Primary sclerosing cholangitis (PSC) is a rare, long-term disease of the liver caused by inflammation of tubes in the liver called bile ducts. Scarring and narrowing of bile ducts leads to liver damage. Over time, the liver loses its ability to filter blood and support digestion.
PSC is rare, affecting up to 1 in 10,000 people. PSC often is linked with inflammatory bowel disease (IBD), especially ulcerative colitis. People with PSC are at higher risk of liver failure and cancers of the bile ducts, gallbladder and colon. Care focuses on monitoring liver health and managing symptoms. Procedures can temporarily open blocked ducts, but liver transplant is the only cure for advanced disease.
Other bile duct conditions may look similar but are different:
- Secondary sclerosing cholangitis develops when another problem, such as infection, gallstones, surgery or injury, damages the bile ducts. It may improve if the cause is treated.
- Pediatric PSC begins in children or teens and can be accompanied by another condition called autoimmune hepatitis.
- Ascending cholangitis is a sudden, dangerous infection of the bile ducts usually caused by a gallstone blockage, and it requires emergency treatment.
Researchers believe PSC is an immune-mediated condition in which the immune system attacks healthy tissues. Another related condition, primary biliary cholangitis, mainly damages the smaller bile ducts inside the liver, occurs mostly in women and often responds to medicines.
Products & Services
Symptoms
About half of people with PSC do not have symptoms when they get a diagnosis. But symptoms appear at some point as damage to the liver worsens.
Symptoms may include:
- Extreme tiredness.
- Itching.
- Pain in the upper belly.
- Diarrhea.
- Fever, related to repeat infections of the bile ducts.
- Yellowing of the whites of the eyes or yellowing of the skin, depending on skin color. This is called jaundice.
When to see a doctor
Make an appointment with your healthcare professional if you have severe, persistent itching on much of your body with no obvious cause. Also, see your health professional if you feel extremely tired all the time, no matter how much rest you get.
It's particularly important to talk with your health professional about extreme tiredness if you have ulcerative colitis or Crohn's disease.
Causes
Primary sclerosing cholangitis (PSC) is an immune-mediated condition. This means the body's immune system attacks its own tissues.
Usually, inflammation is the body's reaction to disease or injury. It increases blood flow, releases proteins that regulate defenses and brings in cells that fight germs. While this process usually helps the body heal, long-term inflammation from an immune-mediated condition can damage tissues.
In PSC, it is not clear what triggers the inflammation of bile ducts. Research shows that PSC likely develops from a combination of factors rather than being passed directly from parent to child, known as simple inheritance. Some people may have a genetic tendency that makes them more vulnerable. On top of this, problems with the immune system and changes in the gut, such as the gut microbiome or environmental exposures, seem to play an important role.
This means that instead of simple inheritance, PSC happens when genetic risk combines with environmental triggers. These may include immune system issues or digestive conditions such as inflammatory bowel disease (IBD). The connection with IBD is strong. About 70% to 80% of people with PSC also have IBD, most often ulcerative colitis. PSC also can occur in people with Crohn's disease, though less commonly.
Risk factors
Factors that may increase the risk of primary sclerosing cholangitis (PSC) include:
- Age. PSC can occur at any age, but it's most often diagnosed in middle-aged adults.
- Sex. PSC occurs more often in men than women.
- Inflammatory bowel disease (IBD). About 5% to 7% of people with some form of IBD, such as ulcerative colitis or Crohn's disease, also have PSC.
- Geographical location. The number of diagnoses of PSC is higher in Northern Europe and North America than in other parts of the world.
- Genes. Certain gene variations may play a role in the risk and development of the disease.
Complications
Complications of PSC may include:
- Liver disease and failure. Long-term inflammation of the bile ducts can lead to damage and scarring of liver tissues, also called cirrhosis. Cirrhosis associated with PSC causes progressive loss of liver function.
- Cancer. There is a significant risk of cancer of the bile ducts and gallbladder. There is less risk of cancer of the liver and pancreas. People with PSC and inflammatory bowel disease have an increased risk of cancer of the colon and rectum.
- Portal hypertension. The portal vein is the major route for blood flowing into the liver. High blood pressure in this vein is called portal hypertension. This complication can cause pressure on blood vessels throughout the digestive system that can lead to internal bleeding. Portal hypertension also can cause fluids from the liver to leak into the cavity holding the digestive organs.
- Bacterial infections. Bacterial infections of the bile ducts may occur, particularly after procedures used to manage the disease or when there is significant blockage of bile ducts.
- Thinning bones. People with PSC may experience thinning bones, also called osteoporosis.
- Vitamin deficiencies. Bile helps the intestines absorb vitamins A, D, E and K. PSC may result in the body not getting enough of these vitamins. This condition is called vitamin deficiency.
Oct. 14, 2025