Diagnosis
Pelvic exam
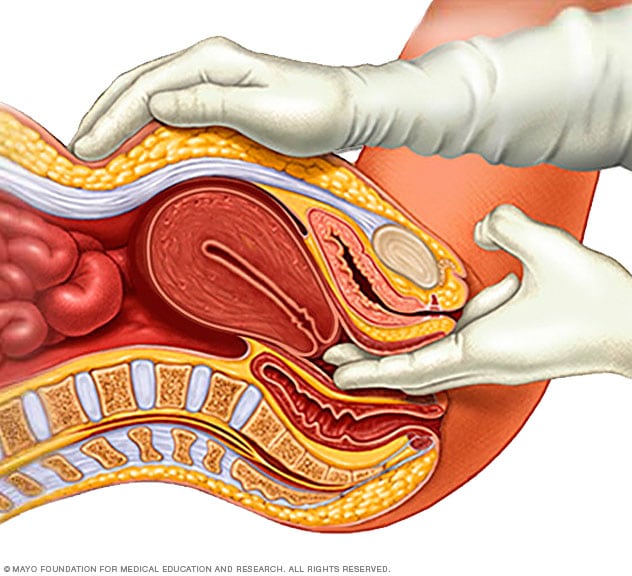
Pelvic exam
During a pelvic exam, a doctor inserts one or two gloved fingers inside the vagina. Pressing down on the abdomen at the same time, the doctor can check the uterus, ovaries and other organs.
Transvaginal ultrasound
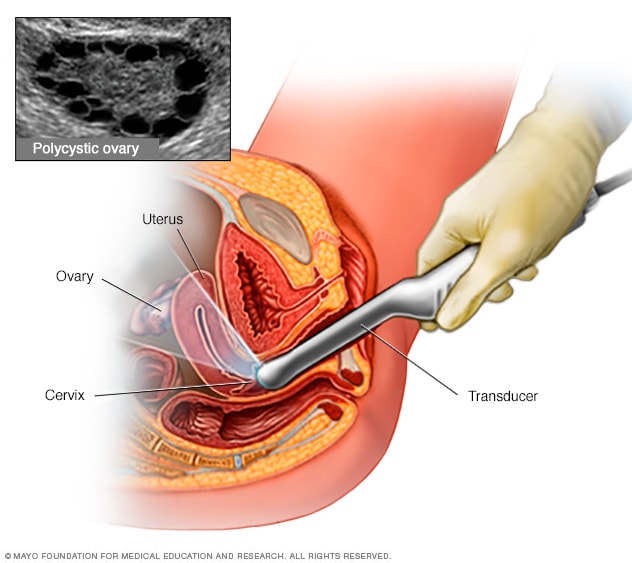
Transvaginal ultrasound
During a transvaginal ultrasound, you lie on your back on an exam table. You have a narrow device, shaped like a wand, inserted into your vagina. This device is called a transducer. The transducer uses sound waves to create images of your ovaries and other pelvic organs. A polycystic ovary has many fluid-filled sacs, called follicles. Each dark circle shown above is one follicle in an ovary.
There's no single test to specifically diagnose polycystic ovary syndrome (PCOS). Your health care provider is likely to start with a discussion of your symptoms, medications and any other medical conditions. Your provider also may ask about your menstrual periods and any weight changes. A physical exam includes checking for signs of excess hair growth, insulin resistance and acne.
Your health care provider might then recommend:
- Pelvic exam. During a pelvic exam, your provider can check your reproductive organs for masses, growths or other changes.
- Blood tests. Blood tests can measure hormone levels. This testing can exclude possible causes of menstrual problems or androgen excess that mimic PCOS. You might have other blood testing, such as fasting cholesterol and triglyceride levels. A glucose tolerance test can measure your body's response to sugar (glucose).
- Ultrasound. An ultrasound can check the appearance of your ovaries and the thickness of the lining of your uterus. A wandlike device (transducer) is placed in your vagina. The transducer emits sound waves that are translated into images on a computer screen.
If you have a diagnosis of PCOS, your provider might recommend more tests for complications. These tests can include:
- Regular checks of blood pressure, glucose tolerance, and cholesterol and triglyceride levels
- Screening for depression and anxiety
- Screening for obstructive sleep apnea
More Information
Treatment
PCOS treatment focuses on managing the things that are concerning you. This could include infertility, hirsutism, acne or obesity. Specific treatment might involve lifestyle changes or medication.
Lifestyle changes
Your health care provider may recommend weight loss through a low-calorie diet combined with moderate exercise activities. Even a modest reduction in your weight — for example, losing 5% of your body weight — might improve your condition. Losing weight may increase the effectiveness of medications your provider recommends for PCOS, and it can help with infertility. Your health care provider and a registered dietitian can work with you to determine the best weight-loss plan.
Medications
To regulate your periods, your health care provider might recommend:
- Combination birth control pills. Pills that contain both estrogen and progestin decrease androgen production and regulate estrogen. Regulating your hormones can lower your risk of endometrial cancer and correct irregular bleeding, excess hair growth and acne.
- Progestin therapy. Taking progestin for 10 to 14 days every 1 to 2 months can regulate your periods and protect against endometrial cancer. This progestin therapy doesn't improve androgen levels and won't prevent pregnancy. The progestin-only minipill or progestin-containing intrauterine device is a better choice if you also wish to avoid pregnancy.
To help you ovulate so that you can become pregnant, your health care provider might recommend:
- Clomiphene. This oral anti-estrogen medication is taken during the first part of your menstrual cycle.
- Letrozole (Femara). This breast cancer treatment can work to stimulate the ovaries.
- Metformin. This medicine for type 2 diabetes that you take by mouth improves insulin resistance and lowers insulin levels. If you don't become pregnant using clomiphene, your provider might recommend adding metformin to help you ovulate. If you have prediabetes, metformin can slow the progression to type 2 diabetes and help with weight loss.
- Gonadotropins. These hormone medications are given by injection.
If needed, talk with your health care provider about procedures that may help you become pregnant. For example, in vitro fertilization may be an option.
To reduce excessive hair growth or improve acne, your health care provider might recommend:
- Birth control pills. These pills decrease androgen production that can cause excessive hair growth and acne.
- Spironolactone (Aldactone). This medication blocks the effects of androgen on the skin, including excessive hair growth and acne. Spironolactone can cause birth defects, so effective birth control is needed while taking this medication. This medication isn't recommended if you're pregnant or planning to become pregnant.
- Eflornithine (Vaniqa). This cream can slow facial hair growth.
- Hair removal. Electrolysis and laser hair removal are two options for removing hair. Electrolysis uses a tiny needle inserted into each hair follicle. The needle sends out a pulse of electric current. The current damages and then destroys the follicle. Laser hair removal is a medical procedure that uses a concentrated beam of light to remove unwanted hair. You might need multiple treatments of electrolysis or laser hair removal. Shaving, plucking or using creams that dissolve unwanted hair may be other options. But these are temporary, and hair may thicken when it grows back.
- Acne treatments. Medications, including pills and topical creams or gels, may help improve acne. Talk to your health care provider about options.
Lifestyle and home remedies
To help ease the effects of PCOS, try to:
- Stay at a healthy weight. Weight loss can lower insulin and androgen levels. It also may restore ovulation. Ask your health care provider about a weight-control program, if you need one. Meet with a registered dietitian for help in reaching weight-loss goals.
- Limit carbohydrates. High-carbohydrate diets might make insulin levels go higher. Ask your provider if a low-carbohydrate diet could help if you have PCOS. Choose complex carbohydrates, which raise your blood sugar levels more slowly. Complex carbohydrates are found in fruits, vegetables, whole grains and cooked dry beans and peas.
- Be active. Exercise helps lower blood sugar levels. If you have PCOS, increasing your daily activity and getting regular exercise may treat or even prevent insulin resistance. Being active may also help you keep your weight under control and avoid developing diabetes.
Preparing for your appointment
For PCOS, you may see a specialist in female reproductive medicine (gynecologist), a specialist in hormone disorders (endocrinologist) or an infertility specialist (reproductive endocrinologist).
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Symptoms you've been having, and for how long
- Information about your periods, including how often they occur, how long they last and how heavy they are
- All medications, vitamins, herbs and other supplements you take, including the dosages
- Key personal and medical information, including other health conditions, recent life changes and stressors
- Questions to ask your health care provider
Some basic questions to ask include:
- What tests do you recommend?
- How does PCOS affect my chance of getting pregnant?
- Are there any medicines that might help improve my symptoms or chance of getting pregnant?
- What lifestyle changes can improve symptoms?
- How will PCOS affect my health in the long term?
- I have other medical conditions. How can I best manage them together?
Don't hesitate to ask other questions as they occur to you.
What to expect from your doctor
Your health care provider is likely to ask you a number of questions, including:
- What are your symptoms? How often do they happen?
- How bad are your symptoms?
- When did each symptom begin?
- When was your last period?
- Have you gained weight since you first started having periods? How much weight did you gain, and when did you gain it?
- Does anything seem to improve your symptoms? Make them worse?
- Are you trying to get pregnant, or do you wish to become pregnant?
- Has any close blood relative, such as your mother or a sister, ever been diagnosed with PCOS?
Sept. 08, 2022