Overview
Patent ductus arteriosus
Patent ductus arteriosus
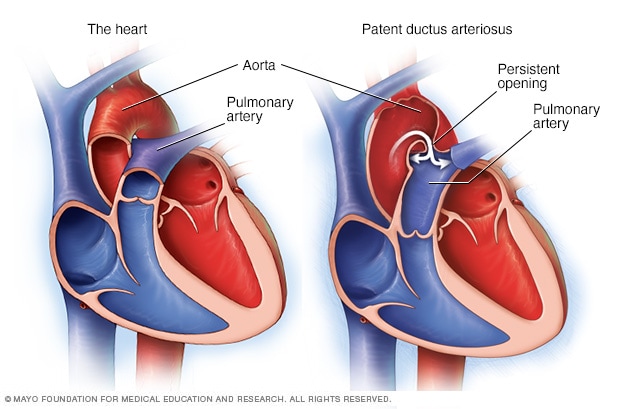
Patent ductus arteriosus is a persistent opening between the two main blood vessels leaving the heart. Those vessels are the aorta and the pulmonary artery. The condition is present at birth.
Patent ductus arteriosus (PDA) is a persistent opening between the two major blood vessels leading from the heart. The heart problem is present from birth. That means it is a congenital heart defect.
An opening called the ductus arteriosus is part of a baby's blood flow system in the womb. It usually closes shortly after birth. If it remains open, it's called a patent ductus arteriosus.
A small patent ductus arteriosus often doesn't cause problems and might never need treatment. However, a large, untreated patent ductus arteriosus can let oxygen-poor blood move the wrong way. This can weaken the heart muscle, causing heart failure and other complications.
Treatment options for a patent ductus arteriosus include regular health checkups, medicines, and a procedure or surgery to close the opening.
Products & Services
Symptoms
Patent ductus arteriosus symptoms (PDA) depend on the size of the opening and the person's age. A small PDA might not cause symptoms. Some people don't notice symptoms until adulthood. A large PDA can cause symptoms of heart failure soon after birth.
A large PDA found during infancy or childhood might cause:
- Poor eating, which leads to poor growth.
- Sweating with crying or eating.
- Persistent fast breathing or breathlessness.
- Easy tiring.
- Rapid heart rate.
When to see a doctor
Contact the doctor if your baby or older child:
- Tires easily when eating or playing.
- Isn't gaining weight.
- Becomes breathless when eating or crying.
- Always breathes rapidly or is short of breath.
Causes
The exact causes of congenital heart defects are unclear. During the first six weeks of pregnancy, a baby's heart starts to form and beat. The major blood vessels to and from the heart grow. It's during this time that certain heart defects may begin to develop.
Before birth, a temporary opening called the ductus arteriosus is between the two main blood vessels leaving a baby's heart. Those vessels are the aorta and the pulmonary artery. The opening is necessary for a baby's blood flow before birth. It moves blood away from a baby's lungs while they develop. The baby gets oxygen from the mother's blood.
After birth, the ductus arteriosus is no longer needed. It usually closes within 2 to 3 days. But in some infants, the opening doesn't close. When it stays open, it's called a patent ductus arteriosus.
The persistent opening causes too much blood to flow to the baby's lungs and heart. Untreated, the blood pressure in the baby's lungs might increase. The baby's heart might grow larger and get weak.
Risk factors
Risk factors for patent ductus arteriosus (PDA) include:
- Premature birth. Patent ductus arteriosus occurs more commonly in babies who are born too early than in babies who are born full term.
- Family history and other genetic conditions. A family history of heart problems present at birth may increase the risk for a PDA. Babies born with an extra 21st chromosome, a condition called Down syndrome, also are more likely to have this condition.
- German measles during pregnancy. Having German measles, also called rubella, during pregnancy can cause problems in a baby's heart development. A blood test done before pregnancy can determine if you're immune to rubella. A vaccine is available for those who aren't immune.
- Being born at a high altitude. Babies born above 8,200 feet (2,499 meters) have a greater risk of a PDA than babies born at lower altitudes.
- Being female. Patent ductus arteriosus is twice as common in girls.
Complications
A small patent ductus arteriosus might not cause complications. Larger, untreated defects could cause:
- High blood pressure in the lungs, also called pulmonary hypertension. A large PDA causes irregular blood flow in the heart and lungs. As a result, pressure rises in the pulmonary artery. Over time, the increased pressure damages the smaller blood vessels in the lungs. A life-threatening and permanent type of lung damage called Eisenmenger syndrome may occur.
- Heart failure. Symptoms of this serious complication include rapid breathing, often with gasping breaths, and poor weight gain.
- Heart infection, called endocarditis. A patent ductus arteriosus can increase the risk of infection of the heart tissue. This infection is called endocarditis. It can be life-threatening.
Patent ductus arteriosus and pregnancy
It may be possible to have a successful pregnancy with a small patent ductus arteriosus. However, having a large PDA or complications such as heart failure, irregular heartbeats or lung damage increases the risk of serious complications during pregnancy.
Before becoming pregnant, talk to your health care provider about possible pregnancy risks and complications. Some heart medicines can cause serious problems for a developing baby. Your health care provider may stop or change your medicines before you become pregnant.
Together you can discuss and plan for any special care needed during pregnancy. If you are at high risk of having a baby with a heart problem present at birth, genetic testing and screening may be done during pregnancy.
Prevention
There is no known prevention for patent ductus arteriosus. However, it's important to do everything possible to have a healthy pregnancy. Here are some of the basics:
- Seek early prenatal care, even before you're pregnant. Quitting smoking, reducing stress, stopping birth control — these are all things to talk to your health care provider about before you get pregnant. Tell your health care provider about all the medicines you take, including those bought without a prescription.
- Eat a healthy diet. Include a vitamin supplement that contains folic acid. Taking 400 micrograms of folic acid daily before and during pregnancy has been shown to reduce brain and spinal cord problems in the baby. It also may help reduce the risk of heart problems.
- Exercise regularly. Work with your health care provider to develop an exercise plan that's right for you.
- Don't drink or smoke. These lifestyle habits can harm a baby's health. Also avoid secondhand smoke.
- Get recommended vaccines. Update your vaccinations before becoming pregnant. Certain types of infections can be harmful to a developing baby.
- Control blood sugar. If you have diabetes, good control of your blood sugar may reduce the risk of certain heart problems before birth.
Jan. 25, 2023