Overview
Occupational asthma is a type of asthma caused by breathing in fumes, gases, dust or other substances while on the job. These substances can trigger an immune system response that changes how the lungs work. Occupational asthma also is called work-related asthma.
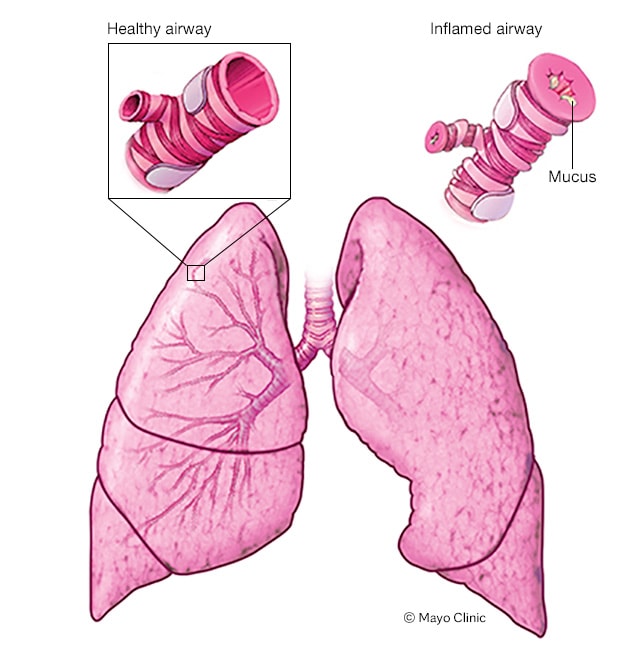
In asthma, the airways narrow and swell. They also may make extra mucus. This makes it difficult to breathe and may cause chest tightness, wheezing and shortness of breath.
Avoiding triggers is important for managing occupational asthma. Treatment includes medicines that reduce symptoms. For people who were diagnosed with asthma in the past, medicines may help improve symptoms related to workplace triggers.
If occupational asthma is not treated and triggers are not avoided, the asthma can cause permanent changes to the lungs.
Products & Services
Symptoms
Asthma attack
Asthma attack
When a person has asthma, the inside walls of the airways in the lungs can narrow and swell. Also, the airway linings may make too much mucus. The result is an asthma attack. During an asthma attack, narrowed airways make breathing difficult and may cause coughing and wheezing.
Occupational asthma symptoms may include:
- Wheezing.
- Coughing.
- Shortness of breath.
- Chest tightness.
Other possible symptoms may include:
- Runny nose.
- Stuffy nose.
- Itchy or watery eyes.
Occupational asthma symptoms depend on the substance you're exposed to, how long and how often you're exposed, and other factors. Your symptoms may:
- Begin right after exposure to a substance, later in the day or after work.
- Improve or go away on days off or during vacations and then return when you go to work.
- May begin early in the day and fail to improve on days off as disease progresses.
- May become permanent even after long periods away from work.
When to see a doctor
Seek medical treatment right away if your symptoms worsen. Severe asthma attacks can be life-threatening. Symptoms of an asthma attack that need emergency treatment include:
- Shortness of breath or wheezing that quickly gets worse.
- No easing of symptoms after using a quick-relief medicine.
- Shortness of breath even with little activity.
Make an appointment to see your healthcare professional if you have breathing problems, such as coughing, wheezing or shortness of breath, especially if the symptoms don't go away or worsen.
Causes
More than 400 workplace substances have been identified as possible triggers of occupational asthma. These substances include:
- Animal proteins found in dander, hair, scales, fur, saliva and body wastes.
- Chemicals used to make paints, varnishes, adhesives, laminates and soldering resin. Other examples include chemicals used to make insulation, packaging materials, and foam mattresses and upholstery.
- Enzymes used in detergents and baking flour.
- Metals, particularly platinum, chromium and nickel sulfate.
- Plant substances, including proteins found in natural rubber latex, flour, cereals, cotton, flax, hemp, rye, wheat and papaya.
- Irritating gases or particles, such as chlorine gas, sulfur dioxide and smoke.
Asthma symptoms start when your lungs become irritated. This irritation causes an immune system reaction called inflammation. Inflammation is defined as swelling and other changes in airway tissues caused by immune system activity. These changes narrow the airways and make it difficult to breathe.
With occupational asthma, lung inflammation may be triggered by a substance that a person is allergic to, such as mold or an animal protein. Sometimes lung inflammation is triggered by an irritating substance, also called an irritant, such as chlorine or smoke.
Risk factors
The more you're exposed to an irritant, the greater the risk of developing occupational asthma. In addition, you will have increased risk if:
- You have existing allergies or asthma. Although this can increase your risk, many people who have allergies or asthma do jobs that expose them to lung irritants and never have symptoms.
- Other family members have allergies or asthma. Your parents may pass down genes that make it more likely for you to develop asthma.
- You work around known asthma triggers. Some substances are known to be lung irritants and asthma triggers.
- You smoke. Smoking increases your risk of developing asthma if you are exposed to certain types of irritants.
High-risk jobs
It's possible to develop occupational asthma in almost any workplace. But your risk is higher in certain workplaces. Some of the riskiest jobs linked to asthma-producing substances include the following:
| Jobs |
Asthma-producing substances |
| Adhesive handlers |
Chemicals |
| Animal handlers, veterinarians |
Animal proteins |
| Bakers, millers, farmers |
Cereal grains |
| Carpet-makers |
Vegetable gums |
| Metalworkers |
Cobalt, nickel |
| Food production workers |
Milk powder, egg powder |
| Forest workers, carpenters, cabinetmakers |
Wood dust |
| Hairdressers |
Dyes |
| Healthcare workers |
Latex and chemicals |
| Pharmaceutical workers, bakers |
Drugs, enzymes |
| Seafood processors |
Herring, snow crab |
| Spray painters, insulation installers, plastics and foam industry workers, welders, metalworkers, chemical manufacturers, shellac handlers |
Chemicals |
| Textile workers |
Dyes, plastics |
| Users of plastics or epoxy resins, chemical manufacturers |
Chemicals |
Complications
The longer you're exposed to a substance that can cause occupational asthma, the worse your symptoms may become. Also, the longer you're exposed, the longer it will take for symptoms to improve after exposure stops. In some cases, exposure to airborne asthma triggers can cause permanent changes to your lungs.
Prevention
The best way to prevent occupational asthma is to control exposure to chemicals and other substances that are known to be irritating. Workplaces can set up controls to prevent exposures, use less harmful substances and provide personal protective equipment (PPE) for workers.
Medicines may help relieve symptoms and control inflammation linked to occupational asthma. But you can do several things on your own to be healthy and lessen the possibility of attacks:
- If you smoke, quit. Being smoke-free may help prevent or lessen symptoms of occupational asthma.
- Get a flu vaccination. This can help prevent illness that affects the lungs.
- Avoid nonsteroidal anti-inflammatory drugs (NSAIDs) and other medicines that may make symptoms worse. Ask your healthcare professional about medicines you take regularly.
- Lose weight. For people with obesity, losing weight can help improve symptoms and overall lung health.
If you are in the United States and you have a high-risk job, your company must follow rules to help protect you from harmful chemicals. Under guidelines from the Occupational Safety and Health Administration (OSHA), your employer is required to do the following:
- Tell you if you'll be working with any harmful chemicals.
- Train you how to safely handle these chemicals.
- Train you how to respond to an emergency, such as a chemical spill.
- Supply protective gear, such as masks and respirators.
- Offer extra training when a new chemical is used at your workplace.
Under OSHA guidelines, your employer is required to keep a material safety data sheet (MSDS) for each harmful chemical used in your workplace. This is a document that must be submitted by the chemical's manufacturer to your employer. You have a legal right to see and copy such documents. If you suspect you're allergic to a certain substance, show the MSDS to your healthcare professional.
While at work, watch for conditions that may not be safe or healthy. Report concerns to your supervisor. If necessary, call OSHA at 800-321-OSHA (800-321-6742) and ask for an on-site inspection. You can do this so that your name won't be revealed to your employer.
Feb. 27, 2024