Overview
Myocarditis
Myocarditis
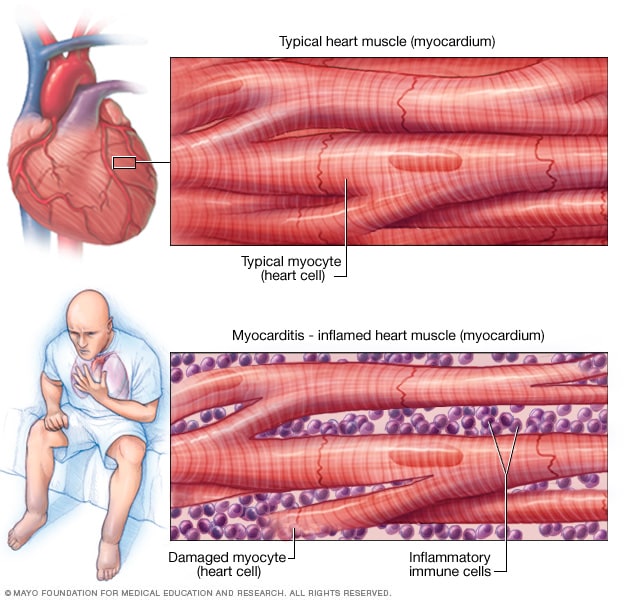
Myocarditis is inflammation of the heart muscle. This illustration shows typical heart muscle compared with damaged heart muscle due to inflammation.
Myocarditis is inflammation of the heart muscle, called the myocardium. The condition can reduce the heart's ability to pump blood. Myocarditis can cause chest pain, shortness of breath, and rapid or irregular heartbeats.
Infection with a virus is one cause of myocarditis. Sometimes myocarditis is caused by a medicine reaction or a condition that causes inflammation throughout the body.
Severe myocarditis weakens the heart so that the rest of the body doesn't get enough blood. Clots can form in the heart, leading to a stroke or heart attack.
Treatment for myocarditis may include medicines, procedures or surgeries.
Symptoms
Some people with early myocarditis don't have symptoms. Others have mild symptoms.
Common myocarditis symptoms include:
- Chest pain.
- Fatigue.
- Swelling of the legs, ankles and feet.
- Rapid or irregular heartbeats, called arrhythmias.
- Shortness of breath, at rest or during activity.
- Lightheadedness or feeling like you might faint.
- Flu-like symptoms such as headache, body aches, joint pain, fever or sore throat.
Sometimes, myocarditis symptoms are like symptoms of a heart attack. If you are having unexplained chest pain and shortness of breath, seek emergency medical help.
Myocarditis in children
When children get myocarditis, symptoms may include:
- Difficulty breathing.
- Rapid breathing.
- Chest pain.
- Rapid or irregular heartbeats, called arrhythmias.
- Fainting.
- Fever.
When to see a doctor
Contact a healthcare professional if you have symptoms of myocarditis. Symptoms of myocarditis can seem like a heart attack. Get emergency medical help if you have unexplained chest pain, rapid heartbeats or shortness of breath.
If you have severe symptoms, go to the emergency room or call for emergency medical help.
Causes
Infections can cause myocarditis.
-
Viruses. Many viruses have been linked to myocarditis, including the adenovirus, which causes the common cold; the COVID-19 virus; viruses that cause hepatitis B and C; parvovirus, which causes a mild rash, usually in children; and herpes simplex virus.
Gastrointestinal infections due to echoviruses, Epstein-Barr virus, which causes mononucleosis, and German measles, also called rubella, all can cause myocarditis. Myocarditis also can be caused by HIV, the virus that causes AIDS.
- Bacteria. Bacteria that can cause myocarditis include staphylococcus, streptococcus, and bacteria that cause diphtheria and Lyme disease.
- Parasites. Parasites that can cause myocarditis are Trypanosoma cruzi and toxoplasma. Some parasites are transmitted by insects and can cause a condition called Chagas disease. Chagas disease is much more common in Central and South America than in the United States.
- Fungi. A fungal infection may cause myocarditis, particularly in people with weakened immune systems. Fungal infections linked to myocarditis include yeast infections, such as candida; molds, such as aspergillus; and histoplasma, often found in bird droppings.
Myocarditis also may be caused by:
- Certain medicines or illegal drugs. These include medicines used to treat cancer; antibiotics, such as penicillin and sulfonamide drugs; some anti-seizure medicines; and cocaine. When these cause myocarditis, it's called drug-induced myocarditis.
- Chemicals or radiation. Exposure to carbon monoxide and radiation can sometimes cause myocarditis.
- Other health conditions. Conditions that may cause myocarditis include lupus, Wegener's granulomatosis, giant cell arteritis and Takayasu's arteritis.
Often, the cause of myocarditis isn't found.
Complications
Usually, myocarditis goes away without complications. However, severe myocarditis can permanently damage the heart muscle.
Possible complications of myocarditis may include:
- Heart failure. Untreated, myocarditis can damage the heart muscle so that it can't pump blood well. People with myocarditis-related heart failure may need a ventricular assist device or a heart transplant.
- Heart attack or stroke. If the heart muscle is damaged and can't pump blood, the blood that collects in the heart can form clots. A heart attack can occur if a clot blocks one of the heart arteries. A stroke can happen if a blood clot in the heart travels to an artery leading to the brain.
- Rapid or irregular heartbeats, called arrhythmias. Damage to the heart muscle can change how the heart beats. Certain arrhythmias increase the risk of stroke.
- Sudden cardiac death. Certain serious irregular heartbeats can cause the heart to suddenly stop beating, a condition called sudden cardiac arrest. If it leads to death it's called sudden cardiac death.
Prevention
There's no specific prevention for myocarditis. However, taking these steps to prevent infections might help:
- Stay away from people who are sick. Stay away from people with symptoms of the flu or other respiratory illness until they are better. If you're sick with symptoms of a viral infection, try to avoid passing the germs to others.
- Wash your hands regularly. Frequent hand-washing is one of the best ways to not get sick and spread germs.
- Avoid risky behaviors. To reduce the chances of getting an HIV-related myocardial infection, practice safe sex and don't use illegal drugs.
- Get recommended vaccines. Stay up to date on recommended vaccines, including those that protect against COVID-19, influenza and rubella — diseases that can cause myocarditis. Rarely, the COVID-19 vaccine can cause myocarditis and inflammation of the outer heart lining, called pericarditis, particularly in males ages 12 to 29. Talk with your healthcare team about the benefits and risks of vaccines.