Overview
A molar pregnancy is a rare complication of pregnancy. It involves unusual growth of cells called trophoblasts. These cells typically become the organ that feeds a growing fetus. That organ also is known as the placenta.
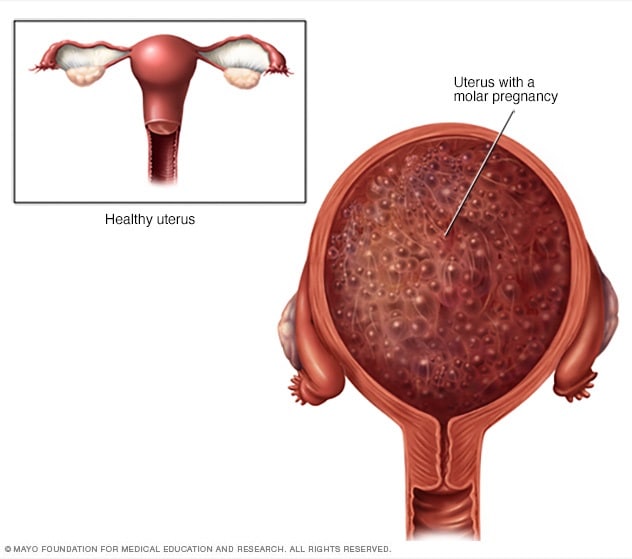
There are two types of molar pregnancy — complete molar pregnancy and partial molar pregnancy. In a complete molar pregnancy, the placental tissue swells and appears to form fluid-filled cysts. There is no fetus.
In a partial molar pregnancy, the placenta might have both regular and irregular tissue. There may be a fetus, but the fetus can't survive. The fetus usually is miscarried early in the pregnancy.
A molar pregnancy can have serious complications, including a rare form of cancer. A molar pregnancy requires early treatment.
Symptoms
Molar pregnancy
Molar pregnancy
During a molar pregnancy, the placenta doesn't form typically. It can look like a mass of cysts. The fetus either doesn't form or doesn't form regularly and can't survive.
A molar pregnancy may seem like a regular pregnancy at first. But most molar pregnancies cause symptoms that can include:
- Dark brown to bright red bleeding from the vagina during the first three months
- Severe nausea and vomiting
- Sometimes grapelike cysts that pass from the vagina
- Pelvic pressure or pain
Because of improved ways of detecting a molar pregnancy, most are found in the first trimester. If it is not found in the first three months, symptoms of a molar pregnancy might include:
- A uterus growing quickly and being too large early in the pregnancy
- Preeclampsia — a condition that causes high blood pressure and protein in the urine — before 20 weeks of pregnancy
- Ovarian cysts
- Overactive thyroid, also known as hyperthyroidism
Causes
An egg fertilized atypically causes a molar pregnancy. Human cells usually have 23 pairs of chromosomes. In a typical fertilization, one chromosome in each pair comes from the father, the other from the mother.
In a complete molar pregnancy, one or two sperm fertilize an egg. The chromosomes from the mother's egg are missing or don't work. The father's chromosomes are copied. There's none from the mother.
In a partial or incomplete molar pregnancy, the mother's chromosomes are present, but the father supplies two sets of chromosomes. The embryo then has 69 chromosomes instead of 46. This most often occurs when two sperm fertilize an egg, resulting in an extra copy of the father's genes.
Risk factors
Factors that can contribute to a molar pregnancy include:
- Earlier molar pregnancy. If you've had one molar pregnancy, you're more likely to have another. A repeat molar pregnancy happens, on average, in 1 out of every 100 people.
- Age of the mother. A molar pregnancy is more likely in people older than age 43 or younger than age 15.
Complications
After removing a molar pregnancy, molar tissue might remain and continue to grow. This is called persistent gestational trophoblastic neoplasia (GTN). GTN happens more often in complete molar pregnancies than it does in partial molar pregnancies.
One sign of persistent GTN is a high level of human chorionic gonadotropin (HCG) — a pregnancy hormone — after the molar pregnancy has been removed. In some cases, the mole that causes the molar pregnancy goes deep into the middle layer of the uterine wall. This causes bleeding from the vagina.
Persistent GTN is usually treated with chemotherapy. Another treatment possibility is removal of the uterus, also known as hysterectomy.
Rarely, a cancerous form of GTN known as choriocarcinoma develops and spreads to other organs. Choriocarcinoma is usually successfully treated with chemotherapy. A complete molar pregnancy is more likely to have this complication than is a partial molar pregnancy.
Prevention
If you've had a molar pregnancy, talk to your pregnancy care provider before trying to get pregnant again. You might want to wait six months to one year. The risk of having another molar pregnancy is low, but it's higher once you've had a molar pregnancy.
During future pregnancies, a care provider may do early ultrasounds to check your condition and make sure the baby is developing.
Dec. 23, 2025