Overview
Leukoplakia
Leukoplakia
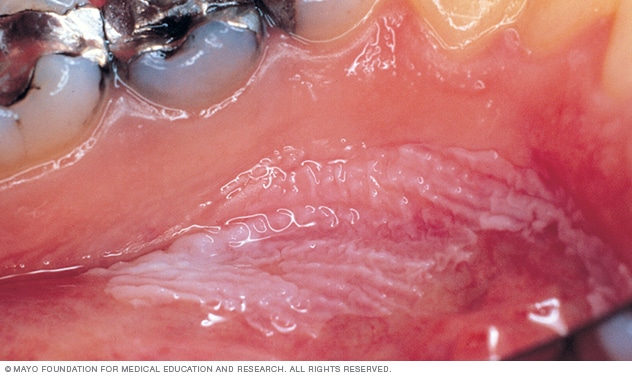
Leukoplakia appears as thick, white patches on the inside surfaces of the mouth. It has several possible causes, including repeated injury or irritation. It also can be a sign of mouth cancer or a sign of changes that could lead to cancer.
Leukoplakia (loo-koh-PLAY-key-uh) causes thick, white patches that form on the gums. The patches also may form on the insides of the cheeks and the bottom of the mouth. Sometimes the patches form on the tongue. These patches cannot be scraped off.
Doctors do not know the exact cause of leukoplakia. But ongoing irritation from tobacco — whether smoked, dipped or chewed — may be the most common cause. Long-term alcohol use is another possible cause.
Most leukoplakia patches are not cancer. But some patches show early signs of cancer. Cancers in the mouth can occur next to areas of leukoplakia. White areas mixed with red areas, also called speckled leukoplakia, may possibly lead to cancer. It's best to see your dentist or doctor if you have any changes in your mouth that do not go away.
A type of leukoplakia in the mouth called hairy leukoplakia mainly affects people whose immune systems have been weakened by disease, especially HIV/AIDS.
Products & Services
Symptoms
Leukoplakia usually occurs on the gums, the insides of the cheeks, the bottom of the mouth under the tongue and, sometimes, the tongue. Usually it is not painful and it may not be noticed for a while.
Leukoplakia may appear as:
- White or gray patches that cannot be wiped away.
- Patches with a rough, ridged, wrinkled or smooth surface, or a combination of these.
- Patches with shapes and edges that are not regular.
- Thick or hard patches.
White patches of leukoplakia may appear along with raised, red areas called erythroplakia (uh-rith-roe-PLAY-key-uh). This combination is called speckled leukoplakia. These patches are more likely to show changes that may lead to cancer.
Hairy leukoplakia
Hairy leukoplakia causes fuzzy, white patches that look like folds or ridges. The patches usually form on the sides of the tongue. Hairy leukoplakia is often mistaken as oral thrush, an infection that causes creamy white patches that can be wiped away. Oral thrush also is common in people with weak immune systems.
When to see a doctor
Even though leukoplakia does not usually cause discomfort, sometimes it can suggest a more serious condition.
See your doctor or other healthcare professional if you have any of these:
- White patches or sores in the mouth that do not heal on their own within two weeks.
- Lumps in the mouth.
- White, red or dark patches in the mouth.
- Changes in the inside of the mouth that do not go away.
- Ear pain.
- Problems swallowing.
- Problems opening the jaw.
Causes
The exact cause of leukoplakia is not known. But long-term irritation from tobacco use — smoked and smokeless — appears to be strongly related to many cases. Often, regular users of smokeless tobacco products get leukoplakia in places where they hold the tobacco between their gums and cheeks.
The use of betel nut, also called an areca nut, may be a cause of leukoplakia. A betel nut packet, like smokeless tobacco, is held between the gum and cheek.
Other possible causes may include ongoing irritation from:
- Long-term, heavy alcohol use.
- Jagged, broken or sharp teeth rubbing on tongue surfaces.
- Broken dentures or dentures that do not fit well.
Your doctor or other healthcare professional can talk with you about what may be causing leukoplakia.
Hairy leukoplakia
Hairy leukoplakia results from infection with the Epstein-Barr virus (EBV). Once you've been infected with EBV, the virus remains in your body for life. Usually the virus is not active and does not cause symptoms. But if your immune system is weakened, especially from HIV/AIDS, the virus can become active. This can lead to conditions such as hairy leukoplakia.
Risk factors
Tobacco use, particularly smokeless tobacco, puts you at high risk of leukoplakia and mouth cancer. Long-term, heavy alcohol use increases your risk. Drinking alcohol combined with using tobacco increases your risk even more.
Hairy leukoplakia
People with HIV/AIDS are especially likely to develop hairy leukoplakia. The use of medicines that slow down or prevent HIV activity has reduced the number of people who get hairy leukoplakia. But it still affects many people who are HIV positive. It may be one of the early signs of HIV infection.
Complications
Leukoplakia usually does not cause permanent damage to the inside of the mouth. But leukoplakia increases the risk of mouth cancer. Mouth cancers often form near leukoplakia patches. And the patches themselves may show cancerous changes. Even after leukoplakia patches are removed, the risk of mouth cancer remains.
Hairy leukoplakia
Hairy leukoplakia is not likely to lead to cancer. But it may be an early symptom of HIV/AIDS.
Prevention
You may be able to prevent leukoplakia if you avoid all tobacco products or alcohol use. Talk to your doctor or other healthcare professional about ways to help you quit. If you continue to smoke or chew tobacco or drink alcohol, have dental checkups often. Mouth cancers are usually painless until advanced. Quitting tobacco and alcohol is a better way to prevent mouth cancers.
Hairy leukoplakia
If you have a weak immune system, you may not be able to prevent hairy leukoplakia. But finding it early can help you get proper treatment.
Feb. 15, 2024