Overview
Left ventricular hypertrophy
Left ventricular hypertrophy
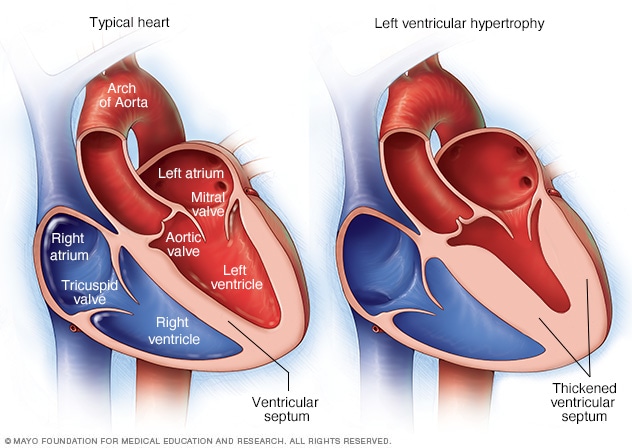
Left ventricular hypertrophy is a thickening of the wall of the heart's main pumping chamber, called the left ventricle. This thickening may increase pressure within the heart. The condition can make it harder for the heart to pump blood. The most common cause is high blood pressure.
Left ventricular hypertrophy is thickening of the walls of the lower left heart chamber. The lower left heart chamber is called the left ventricle. The left ventricle is the heart's main pumping chamber.
During left ventricular hypertrophy, the thickened heart wall can become stiff. Blood pressure in the heart increases. The changes make it harder for the heart to effectively pump blood. Eventually, the heart may fail to pump with as much force as needed.
Uncontrolled high blood pressure is the most common cause of left ventricular hypertrophy. Complications include irregular heart rhythms, called arrhythmias, and heart failure.
Treatment of left ventricular hypertrophy depends on the cause. Treatment may include medications or surgery.
Symptoms
Left ventricular hypertrophy usually develops gradually. Some people do not have symptoms, especially during the early stages of the condition.
Left ventricular hypertrophy itself doesn't cause symptoms. But symptoms may occur as the strain on the heart worsens. They may include:
- Shortness of breath, especially while lying down.
- Swelling of the legs.
- Chest pain, often when exercising.
- Sensation of rapid, fluttering or pounding heartbeats, called palpitations.
- Fainting or a feeling of lightheadedness.
When to see a doctor
Seek emergency care if:
- You feel chest pain that lasts more than a few minutes.
- You have severe difficulty breathing.
- You have severe lightheadedness or lose consciousness.
- You have a sudden, severe headache, difficulty speaking, or weakness on one side of your body.
If you have mild shortness of breath or other symptoms, such as palpitations, see your healthcare professional.
If you have high blood pressure or another condition that increases the risk of left ventricular hypertrophy, your healthcare team is likely to recommend regular health checkups to check your heart.
Causes
Anything that puts stress on the heart's lower left chamber can cause left ventricular hypertrophy. The lower left chamber is called the left ventricle. As the strain on the lower left chamber increases, the muscle tissue in the chamber wall thickens. Sometimes, the size of the heart chamber itself also increases.
Left ventricular hypertrophy also may be caused by gene changes that affect the heart muscle's structure.
Things that can cause the heart to work harder and may possibly lead to left ventricular hypertrophy include:
- High blood pressure. Also called hypertension, this is the most common cause of left ventricular hypertrophy. Long-term high blood pressure strains the left side of the heart, causing it to grow bigger. Treating high blood pressure can help reduce left ventricular hypertrophy symptoms and may even reverse it.
- Narrowing of the aortic valve. The aortic valve is between the lower left heart chamber and the body's main artery, called the aorta. Narrowing of the valve is called aortic stenosis. When the valve is narrowed, the heart must work harder to pump blood into the aorta.
- Intensive athletic training. Intense, long-term strength and endurance training causes changes in the heart. The changes help the heart handle the extra physical workload. But the changes can make the heart muscle grow larger. Sometimes this is called athlete's heart or athletic heart syndrome. It's unclear whether the increased heart size in athletes can lead to stiffening of the heart muscle and disease.
Certain conditions passed down through families, called genetic conditions, can make the heart thicker. They include:
- Hypertrophic cardiomyopathy. This condition is caused by changes in genes that cause the heart muscle to thicken. The thickening makes it harder for the heart to pump blood. It can occur even without high blood pressure. People with one parent with hypertrophic cardiomyopathy have a 50% chance of having the changed gene that causes the disease.
- Amyloidosis. Proteins build up around the organs, including the heart. The collection of proteins interferes with how the organs work. When the condition is passed down through families, it is called familial amyloidosis. It also may affect the nerves and kidneys.
Risk factors
Things that increase the risk of left ventricular hypertrophy include:
- Age. Left ventricular hypertrophy is more common in older people. So is high blood pressure, which can cause heart muscle thickening.
- Weight. Being overweight increases the risk of high blood pressure and left ventricular hypertrophy.
- Family history. Changes in genes passed down through families may lead to left ventricular hypertrophy.
- Diabetes. Having diabetes increases the risk of left ventricular hypertrophy.
- Female gender. Women with high blood pressure are more likely to get the condition than are men with similar blood pressure measurements.
Complications
Left ventricular hypertrophy changes the structure of the heart and how the heart works. The thickened left ventricle becomes weak and stiff. This prevents the lower left heart chamber from filling properly with blood. As a result, blood pressure in the heart increases.
Complications of left ventricular hypertrophy include:
- Heart failure.
- Irregular heart rhythms, called arrhythmias.
- Too little oxygen to the heart, called ischemic heart disease.
- Sudden, unexpected loss of heart function, breathing and consciousness, called sudden cardiac arrest.
Prevention
The same healthy lifestyle changes recommended to treat high blood pressure also help prevent left ventricular hypertrophy. Try these tips:
- Don't smoke.
- Eat healthy foods.
- Use less salt.
- Limit or avoid alcohol.
- Get regular exercise.
- Maintain a healthy weight.
- Get 7 to 9 hours of sleep daily.
- Manage stress.
Uncontrolled high blood pressure increases the risk of left ventricular hypertrophy. Get your blood pressure checked at least every two years if you're 18 and older. If you have risk factors for heart disease or are over age 40, you may need more-frequent checks. Ask your healthcare team what blood pressure reading is best for you. Your healthcare professional may recommend checking your blood pressure at home. Home blood pressure monitors are available at local stores and pharmacies.
The Mayo Clinic experience and patient stories
Our patients tell us that the quality of their interactions, our attention to detail and the efficiency of their visits mean health care like they've never experienced. See the stories of satisfied Mayo Clinic patients.
Aug. 06, 2024