Overview
Invasive lobular carcinoma is a type of breast cancer that begins as a growth of cells in the milk-producing glands of the breast. These glands are called lobules.
Invasive cancer means that the cancer cells have broken out of the lobule where they began and spread into the breast tissue. The cells have the potential to spread to the lymph nodes and other areas of the body.
Invasive lobular carcinoma makes up a small portion of all breast cancers. The most common type of breast cancer begins in the breast ducts. This type is called invasive ductal carcinoma.
Products & Services
Symptoms
At first, invasive lobular carcinoma may cause no signs and symptoms. As it grows larger, invasive lobular carcinoma may cause:
- A change in the texture or appearance of the skin over the breast, such as dimpling or thickening.
- A new area of fullness or swelling in the breast.
- A newly inverted nipple.
- An area of thickening in part of the breast.
Invasive lobular carcinoma is less likely to cause a firm or distinct breast lump than other types of breast cancer.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you notice a change in your breasts. Changes to look for may include a lump, an area of puckered or otherwise unusual skin, a thickened region under the skin, and nipple discharge.
Ask your healthcare professional when you should consider breast cancer screening and how often it should be repeated. Most healthcare professionals recommend considering routine breast cancer screening beginning in your 40s.
Causes
Breast anatomy
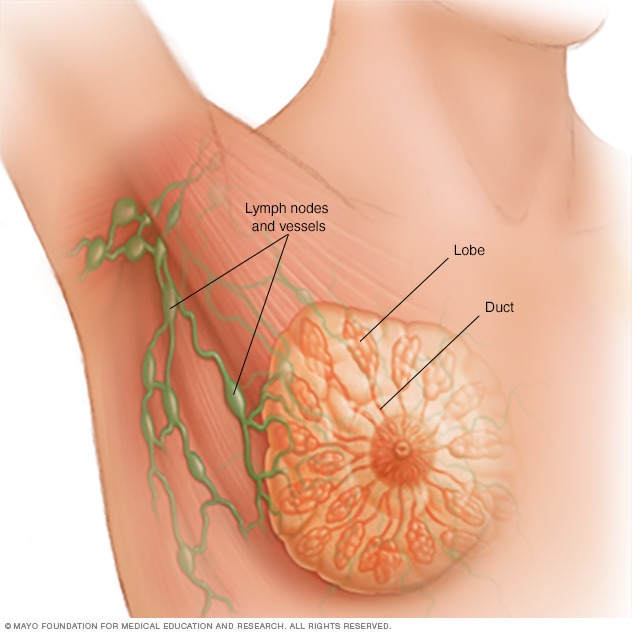
Breast anatomy
Each breast contains 15 to 20 lobes of glandular tissue, arranged like the petals of a daisy. The lobes are further divided into smaller lobules that produce milk for breastfeeding. Small tubes, called ducts, conduct the milk to a reservoir that lies just beneath the nipple.
It's not clear what causes invasive lobular carcinoma.
This form of breast cancer begins when cells in one or more milk-producing glands of the breast develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
Invasive lobular carcinoma cells tend to invade breast tissue by spreading out rather than forming a firm lump. The affected area may have a different feel from the surrounding breast tissue. The area may feel more like a thickening and fullness, but it's unlikely to feel like a lump.
Risk factors
Risk factors for invasive lobular carcinoma are thought to be similar to the risk factors for breast cancer in general. Factors that may increase the risk of breast cancer include:
- A family history of breast cancer. If a parent, sibling or child had breast cancer, your risk of breast cancer is increased. The risk is higher if your family has a history of getting breast cancer at a young age. The risk also is higher if you have multiple family members with breast cancer. Still, most people diagnosed with breast cancer don't have a family history of the disease.
- A personal history of breast cancer. If you've had cancer in one breast, you have an increased risk of getting cancer in the other breast.
- A personal history of breast conditions. Certain breast conditions are signs that you have a higher risk of breast cancer. These conditions include lobular carcinoma in situ, also called LCIS, and atypical hyperplasia of the breast. If you've had a breast biopsy that found one of these conditions, you have an increased risk of breast cancer.
- Beginning your period at a younger age. Beginning your period before age 12 increases your risk of breast cancer.
- Beginning menopause at an older age. Beginning menopause after age 55 increases the risk of breast cancer.
- Being female. Women are much more likely than men are to get breast cancer. Everyone is born with some breast tissue, so anyone can get breast cancer.
- Dense breast tissue. Breast tissue is made up of fatty tissue and dense tissue. Dense tissue is made of milk glands, milk ducts and fibrous tissue. If you have dense breasts, you have more dense tissue than fatty tissue in your breasts. Having dense breasts can make it harder to detect breast cancer on a mammogram. If a mammogram showed that you have dense breasts, your risk of breast cancer is increased. Talk with your healthcare team about other tests you might have in addition to mammograms to look for breast cancer.
- Drinking alcohol. Drinking alcohol increases the risk of breast cancer.
- Having your first child at an older age. Giving birth to your first child after age 30 may increase the risk of breast cancer.
- Having never been pregnant. Having been pregnant one or more times lowers the risk of breast cancer. Never having been pregnant increases the risk.
- Inherited DNA changes that increase cancer risk. Certain DNA changes that increase the risk of breast cancer can be passed from parents to children. Two DNA changes associated with an increased risk of invasive lobular carcinoma include BRCA2 and CDH1. BRCA2 increases the risk of breast cancer and ovarian cancer. CDH1 increases the risk of breast cancer and stomach cancer. CDH1 is closely associated with a rare inherited condition called hereditary diffuse gastric cancer syndrome.
- Menopausal hormone therapy. Taking certain hormone therapy medicines to control the symptoms of menopause may increase the risk of breast cancer. The risk is linked to hormone therapy medicines that combine estrogen and progesterone. The risk goes down when you stop taking these medicines.
- Obesity. People with obesity have an increased risk of breast cancer.
- Older age. Your risk of breast cancer increases as you age. Invasive lobular carcinoma tends to happen at an older age compared to other types of breast cancer.
- Radiation exposure. If you received radiation treatments to your chest as a child or young adult, your risk of breast cancer is higher.
Prevention
Making changes in your daily life may help lower your risk of invasive lobular carcinoma and other types of breast cancer. Try to:
Ask about breast cancer screening
Talk with your doctor or other healthcare professional about when to begin breast cancer screening. Ask about the benefits and risks of screening. Together, you can decide what breast cancer screening tests are right for you.
Become familiar with your breasts through breast self-exam
You may choose to become familiar with your breasts by occasionally inspecting them during a breast self-exam for breast awareness. If there is a new change, a lump or something not typical in your breasts, report it to a healthcare professional right away.
Breast awareness can't prevent breast cancer. But it may help you to better understand the look and feel of your breasts. This might make it more likely that you'll notice if something changes.
Drink alcohol in moderation, if at all
If you choose to drink alcohol, limit the amount you drink to no more than one drink a day. For breast cancer prevention, there is no safe amount of alcohol. So if you're very concerned about your breast cancer risk, you may choose to not drink alcohol.
Exercise most days of the week
Aim for at least 30 minutes of exercise on most days of the week. If you haven't been active lately, ask a healthcare professional whether it's OK and start slowly.
Limit menopausal hormone therapy
Combination hormone therapy may increase the risk of breast cancer. Talk with a healthcare professional about the benefits and risks of hormone therapy.
Some people have symptoms during menopause that cause discomfort. These people may decide that the risks of hormone therapy are acceptable in order to get relief. To reduce the risk of breast cancer, use the lowest dose of hormone therapy possible for the shortest amount of time.
Maintain a healthy weight
If your weight is healthy, work to maintain that weight. If you need to lose weight, ask a healthcare professional about healthy ways to lower your weight. Eat fewer calories and slowly increase the amount of exercise.
Talk with a healthcare professional about your cancer risk
If you have a family history of breast cancer or feel that you may have an increased risk of breast cancer, talk about it with your healthcare professional. Preventive medicines, surgery and more-frequent screening may be options for people with a high risk of breast cancer.