Overview
Digestive system
Digestive system
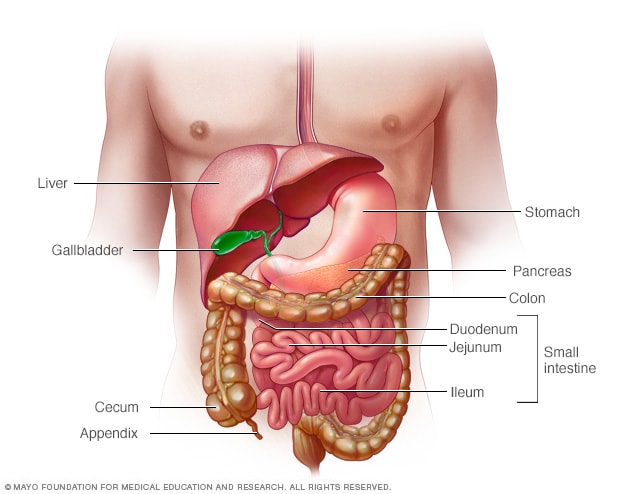
In Crohn's disease, any part of your small or large intestine can be involved. It may involve multiple segments, or it may be continuous. Crohn's disease most commonly affects the last part of the small intestine (ileum) and parts of the colon.
Gastroenterology & GI Surgery Blog
Connect with others and follow the latest advances in treating Crohn's disease and ulcerative colitis on Mayo Clinic Connect.
Inflammatory bowel disease (IBD) is a term that describes disorders involving long-standing (chronic) inflammation of tissues in your digestive tract. Types of IBD include:
- Ulcerative colitis. This condition involves inflammation and sores (ulcers) along the lining of your large intestine (colon) and rectum.
- Crohn's disease. This type of IBD is characterized by inflammation of the lining of your digestive tract, which often can involve the deeper layers of the digestive tract. Crohn's disease most commonly affects the small intestine. However, it can also affect the large intestine and uncommonly, the upper gastrointestinal tract.
Both ulcerative colitis and Crohn's disease usually are characterized by diarrhea, rectal bleeding, abdominal pain, fatigue and weight loss.
For some people, IBD is only a mild illness. For others, it's a debilitating condition that can lead to life-threatening complications.
Products & Services
Symptoms
Inflammatory bowel disease symptoms vary, depending on the severity of inflammation and where it occurs. Symptoms may range from mild to severe. You are likely to have periods of active illness followed by periods of remission.
Signs and symptoms that are common to both Crohn's disease and ulcerative colitis include:
- Diarrhea
- Fatigue
- Abdominal pain and cramping
- Blood in your stool
- Reduced appetite
- Unintended weight loss
When to see a doctor
See your doctor if you experience a persistent change in your bowel habits or if you have any of the signs and symptoms of inflammatory bowel disease. Although inflammatory bowel disease usually isn't fatal, it's a serious disease that, in some cases, may cause life-threatening complications.
Causes
The exact cause of inflammatory bowel disease remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but aren't the cause of IBD.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an atypical immune response causes the immune system to attack the cells in the digestive tract, too.
Several gene mutations have been associated with IBD. Heredity also seems to play a role in that IBD is more common in people who have family members with the disease. However, most people with IBD don't have this family history.
Risk factors
- Age. Most people who develop IBD are diagnosed before they're 30 years old. But some people don't develop the disease until their 50s or 60s.
- Race or ethnicity. Although IBD is more common in white people, it can occur in any race. Cases are also increasing in other races and ethnicities.
- Family history. You're at higher risk if you have a close relative — such as a parent, sibling or child — with the disease.
-
Cigarette smoking. Cigarette smoking is the most important controllable risk factor for developing Crohn's disease.
Smoking may help prevent ulcerative colitis. However, its harm to overall health outweighs any benefit, and quitting smoking can improve the general health of your digestive tract, as well as provide many other health benefits.
- Nonsteroidal anti-inflammatory medications. These include ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve), diclofenac sodium and others. These medications may increase the risk of developing IBD or worsen the disease in people who have IBD.
Complications
Ulcerative colitis and Crohn's disease have some complications in common and others that are specific to each condition. Complications found in both conditions may include:
- Colon cancer. Having ulcerative colitis or Crohn's disease that affects most of your colon can increase your risk of colon cancer. Screening for cancer with a colonoscopy at regular intervals begins usually about 8 to 10 years after the diagnosis is made. Ask your doctor when and how frequently you need to have this test done.
- Skin, eye and joint inflammation. Certain disorders, including arthritis, skin lesions and eye inflammation (uveitis), may occur during IBD flare-ups.
- Medication side effects. Certain medications for IBD are associated with a risk of infections. Some carry a small risk of developing certain cancers. Corticosteroids can be associated with a risk of osteoporosis, high blood pressure and other conditions.
- Primary sclerosing cholangitis. In this rather uncommon condition seen in people with IBD, inflammation causes scarring within the bile ducts. This scarring eventually narrows the ducts, restricting bile flow. This can eventually cause liver damage.
- Blood clots. IBD increases the risk of blood clots in veins and arteries.
- Severe dehydration. Excessive diarrhea can result in dehydration.
Complications of Crohn's disease may include:
- Bowel obstruction. Crohn's disease affects the full thickness of the intestinal wall. Over time, parts of the bowel can thicken and narrow, which may block the flow of digestive contents. You may require surgery to remove the diseased portion of your bowel.
- Malnutrition. Diarrhea, abdominal pain and cramping may make it difficult for you to eat or for your intestine to absorb enough nutrients to keep you nourished. It's also common to develop anemia due to low iron or vitamin B-12 caused by the disease.
- Fistulas. Sometimes inflammation can extend completely through the intestinal wall, creating a fistula — an atypical connection between different body parts. Fistulas near or around the anal area (perianal) are the most common kind. But they can also occur internally or toward the wall of the abdominal area. In some cases, a fistula may become infected and form an infected pocket of pus known as an abscess.
- Anal fissure. This is a small tear in the tissue that lines the anus or in the skin around the anus where infections can occur. It's often associated with painful bowel movements and may lead to a perianal fistula.
Complications of ulcerative colitis may include:
- Toxic megacolon. Ulcerative colitis may cause the colon to rapidly widen and swell, a serious condition known as toxic megacolon.
- A hole in the colon (perforated colon). A perforated colon most commonly is caused by toxic megacolon, but it may also occur on its own.
Sept. 03, 2022