Diagnosis
Transvaginal ultrasound
Transvaginal ultrasound
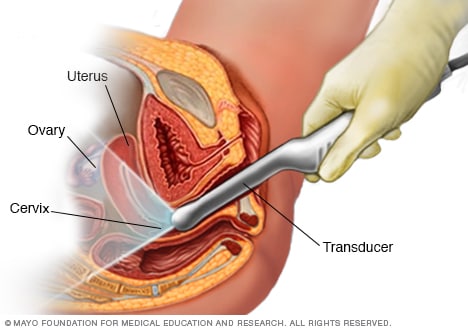
During a transvaginal ultrasound, a healthcare professional or technician uses a wandlike device called a transducer. The transducer is inserted into your vagina while you lie on your back on an exam table. The transducer emits sound waves that generate images of your pelvic organs.
An incompetent cervix can be found only during pregnancy. It can be a difficult diagnosis to make, especially during a first pregnancy.
Your doctor or other member of your care team may ask about your symptoms and medical history. Be sure to tell your care team if you've had a pregnancy loss in the second trimester of a past pregnancy or if you have a history of preterm delivery. Also tell your care team about any procedures you've had on your cervix.
Your doctor might diagnose an incompetent cervix if you have:
- A history of painless widening of the cervix, known as dilation, and second trimester delivery during a past pregnancy.
- Advanced cervical dilation and effacement before week 24 of pregnancy. Effacement means the cervix gets thinner and softer. Cervical dilation and effacement can happen without painful contractions. They may also happen with vaginal bleeding, infection or ruptured membranes, which is when your water breaks.
Diagnosis of an incompetent cervix during the second trimester also may include:
- An ultrasound exam. During this exam, you have a thin, wandlike device, called a transducer, placed inside the vagina. This is known as a transvaginal ultrasound. The transducer puts out sound waves that get converted to pictures you can see on a screen. This type of ultrasound can be used to check the length of your cervix and to see if any tissues are sticking out of the cervix.
- A pelvic exam. During a pelvic exam, your doctor checks the cervix to see if the amniotic sac can be felt through the opening. The amniotic sac is where the baby is growing. If the wall of the sac is in the cervical canal or vagina, it's called prolapsed fetal membranes, and it means that the cervix has started to open. Your doctor may also check to see if you're having any contractions and track them, if needed.
- Lab tests. If you have prolapsed fetal membranes, you may need other tests to rule out an infection. In some cases, this may include taking a sample of amniotic fluid. This is called an amniocentesis. Amniocentesis can be used to check for infection in the amniotic sac and fluid.
There are no reliable tests that can be done before pregnancy to predict if you'll have an incompetent cervix. But certain tests done before pregnancy, such as an ultrasound or MRI, could help find congenital problems with the uterus that might cause an incompetent cervix.
More Information
Treatment
Cervical cerclage

Cervical cerclage
In a cervical cerclage, strong stiches, called sutures, are used to close the cervix during pregnancy to help prevent premature birth. Often, the stitches are removed during the last month of pregnancy.
Treatment options or ways to manage an incompetent cervix include:
- Progesterone supplementation. If you have a short cervix with no history of a preterm birth, vaginal progesterone may lower your risk of having your baby too early. This medicine comes in the form of a gel or a suppository that gets placed in the vagina each day.
- Repeated ultrasounds. If you have a history of early premature birth, or a history that may increase your risk of an incompetent cervix, your doctor might closely monitor the length of your cervix. To do this, you have ultrasounds every two weeks from week 16 through week 24 of pregnancy. If your cervix begins to open or becomes shorter than a certain length, you might need a cervical cerclage.
-
Cervical cerclage. During this procedure, the cervix is stitched tightly closed. The stitches are taken out during the last month of pregnancy or just before delivery. You may need a cervical cerclage if you are less than 24 weeks pregnant, you have a history of early births and an ultrasound shows that your cervix is starting to open.
Sometimes, cervical cerclage is done as a preventive measure before the cervix starts to open. This is known as a prophylactic cervical cerclage. You might have this type of cervical cerclage if you've had an incompetent cervix with past pregnancies. This procedure often is done before 14 weeks of pregnancy.
Cervical cerclage isn't the right choice for everyone at risk of premature birth. For instance, the procedure isn't recommended if you're pregnant with twins or more. Be sure to talk to your doctor about the risks and benefits cervical cerclage may have for you.
- Pessary. A device called a pessary fits inside the vagina and holds the uterus in place. A pessary may help lessen pressure on the cervix. But more research is needed to see if a pessary will work well for treating an incompetent cervix.
Lifestyle and home remedies
If you have an incompetent cervix, your doctor might suggest limiting sexual activity or avoiding certain other physical activities. This advice will depend on your individual situation.
Coping and support
It may be difficult to learn that you have an incompetent cervix. It may make you feel anxious about your pregnancy and afraid to think about the future. Ask your care team for suggestions on safe ways to relax.
Having a premature birth might make you feel that you did something to cause it. Or that you could have done more to stop it from happening. If you're struggling with these feelings, talk to your partner and loved ones, as well as your doctor. Try to focus your energy on caring for and getting to know your baby.
Preparing for your appointment
Tell your doctor about any risk factors you may have for an incompetent cervix. Also tell your doctor if you have any symptoms during your second trimester that might mean you have an incompetent cervix. Depending on the situation, you might need immediate medical care.
Here's some information to help you get ready for your appointment, as well as what to expect from your health care provider.
What you can do
If there's time before your appointment, you might want to:
- Find a loved one or friend who can join you for your appointment. Worry and anxiety might make it hard to pay attention to what your doctor says. Take someone along who can help you remember what you talked about during your appointment.
- Write down questions to ask your health care team. That way, you won't forget anything important that you want to ask. This can help you make the most of your time with your doctor.
Basic questions to ask your doctor about problems with the cervix during pregnancy include:
- Has my cervix begun to open? If so, how much?
- Is there anything I can do to help continue my pregnancy?
- Are there any treatments that can make my pregnancy last longer or help the baby?
- Do I need to be on bed rest? If so, for how long? What kinds of things will I be able to do? Will I need to be in the hospital?
- What warning signs should make me call you?
- What warning signs should make me to go to the hospital?
- If my baby is born now, what can I expect?
Feel free to ask any other questions that occur to you.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- When did your symptoms start?
- Have you had any contractions?
- Have you noticed changes in vaginal discharge?
- Have you had any earlier pregnancies, miscarriages or cervical surgeries that you haven't mentioned?
- How long would it take you to get to the hospital in an emergency, including time to arrange child care or a ride to the hospital?
- Do you have friends or family nearby who could care for you if you need bed rest?