Diagnosis
During the physical exam, your health care professional will check your back for tenderness. You might be asked to lie flat and move your legs into various positions to help determine the cause of your pain.
Your doctor also may perform a neurological exam to check your:
- Reflexes.
- Muscle strength.
- Walking ability.
- Ability to feel light touches, pinpricks or vibration.
In most cases of herniated disk, a physical exam and a medical history are all that are needed for a diagnosis. If your health care professional suspects another condition or needs to see which nerves are affected, you may have one or more of the following tests.
Imaging tests
- X-rays. Plain X-rays don't detect herniated disks, but they can rule out other causes of back pain. X-rays can show an infection, a tumor, spinal alignment issues or a broken bone.
- CT scan. A CT scanner takes a series of X-rays from different directions. Those images are combined to create cross-sectional images of the spinal column and the structures around it.
- MRI. Radio waves and a strong magnetic field are used to create images of the body's inner structures. This test can be used to confirm the location of the herniated disk and to see which nerves are affected.
- Myelogram. A dye is injected into the spinal fluid before a CT scan is done. This test can show pressure on the spinal cord or nerves due to multiple herniated disks or other conditions.
Nerve tests
Nerve conduction studies and electromyograms (EMGs) measure how well electrical impulses are moving along nerve tissue. This can help pinpoint the location of nerve damage.
- Nerve conduction study. This test measures electrical nerve impulses and functioning in the muscles and nerves through electrodes placed on the skin. The study measures the electrical impulses in nerve signals when a small current passes through the nerve.
- Electromyogram (EMG). During an EMG, a doctor inserts a needle electrode through the skin into various muscles. The test evaluates the electrical activity of muscles when contracted and when at rest.
More Information
Treatment
Conservative treatment includes changing activities to stay away from movement that causes pain and taking pain medicines. This treatment relieves symptoms in most people within a few days or weeks.
Medications
- Nonprescription pain medicines. If your pain is mild to moderate, your health care professional might recommend nonprescription pain medicine. Options include acetaminophen (Tylenol, others) ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve).
- Neuropathic drugs. These drugs affect nerve impulses to decrease pain. They include gabapentin (Horizant, Neurontin), pregabalin (Lyrica), duloxetine (Cymbalta), or venlafaxine (Effexor XR).
- Muscle relaxers. You might be prescribed these if you have muscle spasms. Sedation and dizziness are common side effects.
- Opioids. Because of the side effects of opioids and the potential for addiction, many health care professionals hesitate to prescribe them for disk herniation. If other medicines don't relieve your pain, your health care professional might consider short-term use of opioids. Codeine or an oxycodone-acetaminophen combination (Percocet) may be used. Sedation, nausea, confusion and constipation are possible side effects of these medicines.
- Cortisone injections. If your pain doesn't improve with oral medicines, your health care professional might recommend a corticosteroid injection. This medicine can be injected into the area around the spinal nerves. Spinal imaging can help guide the needle.
Therapy
Your health care team might suggest physical therapy to help with your pain. Physical therapists can show you positions and exercises designed to minimize the pain of a herniated disk.
Surgery
Diskectomy
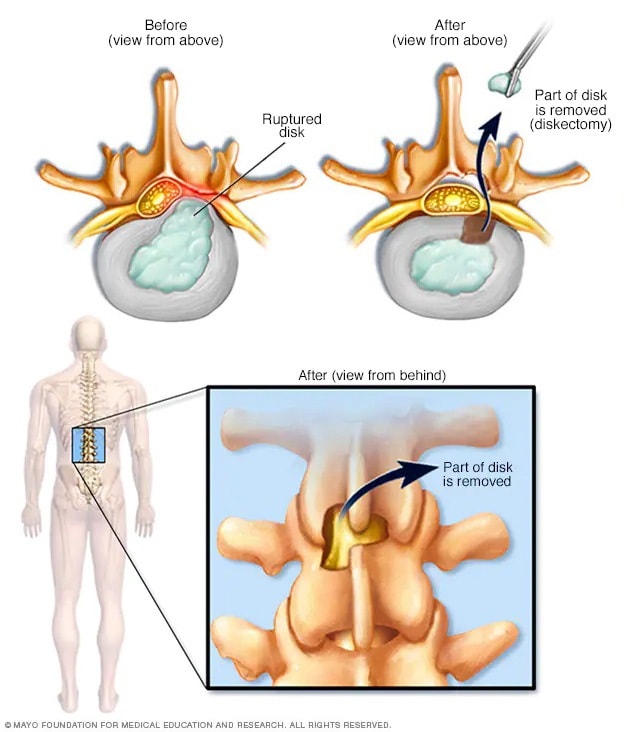
Diskectomy
Diskectomy is the surgical removal of the damaged portion of a herniated disk in the spine. A herniated disk occurs when some of the softer material inside the disk pushes out through a crack in the tougher outside of the disk. This can irritate or press on nearby nerves and cause pain, numbness or weakness.
Few people with herniated disks require surgery. If conservative treatments fail to improve your symptoms after six weeks, surgery may be an option, especially if you continue to have:
- Poorly controlled pain.
- Numbness or weakness.
- Trouble standing or walking.
- Loss of bladder or bowel control.
In nearly all cases, surgeons can remove just the protruding portion of the disk. Rarely, the entire disk must be removed. In these cases, the vertebrae might need to be fused with a bone graft.
To allow the process of bone fusion, which takes months, metal hardware is placed in the spine to provide spinal stability. Rarely, your surgeon might suggest the implantation of an artificial disk.
More Information
Lifestyle and home remedies
Besides taking the pain medicines your health care professional recommends, try:
- Applying heat or cold. At first, cold packs can be used to relieve pain and swelling. After a few days, you might switch to gentle heat to give relief and comfort.
- Avoiding too much bed rest. Staying in bed can lead to stiff joints and weak muscles — which can complicate your recovery. Instead, rest in a position of comfort for 30 minutes, and then go for a short walk or do some work. Try to avoid activities that worsen your pain.
- Resuming activity slowly. Let your pain guide you in resuming your activities. Make sure your movements are slow and controlled, especially bending forward and lifting.
Alternative medicine
Some alternative and complementary medicine treatments might help ease chronic back pain. Examples include:
- Chiropractic. Spinal manipulation has been found to be moderately effective for low back pain that has lasted for at least a month. Rarely, chiropractic treatment of the neck can cause certain types of strokes.
- Acupuncture. Although results are usually modest, acupuncture appears to ease chronic back and neck pain.
- Massage. This hands-on therapy can provide short-term relief to people dealing with chronic low back pain.
Preparing for your appointment
You're likely to start by seeing your family health care professional. You might be referred to a specialist in physical medicine and rehabilitation, orthopedic surgery, neurology, or neurosurgery.
What you can do
Before your appointment, be prepared to answer the following questions:
- When did your symptoms start?
- Were you lifting, pushing or pulling anything at the time you first felt symptoms? Were you twisting your back?
- Has the pain kept you from taking part in activities?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- What medicines or supplements do you take?
What to expect from your doctor
Your health care team might ask other questions, including:
- Does your pain travel into your arms or legs?
- Do you feel weakness or numbness in your arms or legs?
- Have you noticed changes in your bowel or bladder habits?
- Does coughing or sneezing worsen your pain?
- Is the pain interfering with sleep or work?
- Does your work involve heavy lifting?
- Do you smoke or use other tobacco products?
- How has your weight changed recently?