Overview
A herniated disk refers to a problem with one of the rubbery cushions, called disks, that sit between the bones that stack to make the spine. These bones are called vertebrae.
A spinal disk has a soft, jellylike center called a nucleus. The nucleus is encased in a tougher, rubbery exterior, known as the annulus. A herniated disk occurs when some of the nucleus pushes out through a tear in the annulus. A herniated disk is sometimes called a slipped disk or a ruptured disk.
A herniated disk, which can occur in any part of the spine, most often occurs in the lower back. Depending on where the herniated disk is, it can result in pain, numbness or weakness in an arm or a leg.
Many people have no symptoms from a herniated disk. For people who do have symptoms, the symptoms tend to improve over time. Surgery is usually not needed to relieve the problem.
Herniated disk
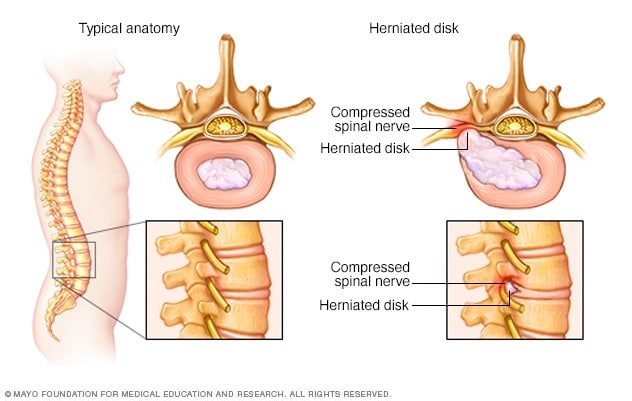
Herniated disk
The disks that lie between the vertebrae in the spine consist of a soft center (nucleus) surrounded by a tougher exterior (annulus). A herniated disk occurs when a portion of the nucleus pushes through a crack in the annulus. Symptoms may occur if the herniation compresses a nerve.
Products & Services
Symptoms
Most herniated disks occur in the lower back, but they also can occur in the neck. Symptoms depend on where the disk is sitting and whether the disk is pressing on a nerve. Herniated disks often affect one side of the body.
-
Arm or leg pain. If your herniated disk is in your lower back, you'll typically feel pain in your lower back, buttocks, thigh and calf. You might have pain in part of your foot as well.
For a herniated disk in your neck, you'll typically feel the most pain in your shoulder and arm. This pain might shoot into your arm or leg when you cough, sneeze or move into certain positions. Pain is often described as sharp or burning.
- Numbness or tingling. People who have herniated disks often have radiating numbness or tingling in the body part served by the affected nerves.
- Weakness. Muscles served by the affected nerves tend to weaken. This can cause you to stumble or affect your ability to lift or hold items.
You can have a herniated disk without symptoms. You might not know you have it unless it shows up on a spinal image.
When to see a doctor
Seek medical care if your neck or back pain travels down your arm or leg, or if you also have numbness, tingling or weakness.
Causes
Disk herniation is most often the result of a gradual, aging-related wear and tear called disk degeneration. As people age, the disks become less flexible and more prone to tearing or rupturing with even a minor strain or twist.
Most people can't pinpoint the cause of their herniated disk. Sometimes, using the back muscles instead of the leg and thigh muscles to lift heavy objects can lead to a herniated disk. Twisting and turning while lifting also can cause a herniated disk. Rarely, a traumatic event such as a fall or a blow to the back is the cause.
Risk factors
Factors that can increase the risk of a herniated disk include:
- Weight. Excess body weight causes extra stress on the disks in the lower back.
- Occupation. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways and twisting also can increase the risk of a herniated disk.
- Genetics. Some people inherit a predisposition to developing a herniated disk.
- Smoking. It's thought that smoking lessens the oxygen supply to disks, causing them to break down more quickly.
- Frequent driving. Being seated for long periods combined with the vibration from a motor vehicle engine can put pressure on the spine.
- Being sedentary. Regular exercise can help prevent a herniated disk.
Complications
Just above your waist, your spinal cord ends. What continues through the spinal canal is a group of long nerve roots that resembles a horse's tail, called the cauda equina.
Rarely, disk herniation can compress the entire spinal canal, including all the nerves of the cauda equina. In rare instances, emergency surgery might be needed to avoid permanent weakness or paralysis.
Seek emergency medical attention if you have:
- Worsening symptoms. Pain, numbness or weakness can increase to the point that they hamper your daily activities.
- Bladder or bowel dysfunction. Cauda equina syndrome can cause incontinence or trouble urinating even with a full bladder.
- Saddle anesthesia. This progressive loss of sensation affects the areas that would touch a saddle — the inner thighs, the backs of the legs and the area around the rectum.
Prevention
To help prevent a herniated disk, do the following:
- Exercise. Strengthening the trunk muscles stabilizes and supports the spine.
- Maintain good posture. This reduces pressure on your spine and disks. Keep your back straight and aligned, particularly when sitting for long periods. Lift heavy objects properly, making your legs — not your back — do most of the work.
- Maintain a healthy weight. Excess weight puts more pressure on the spine and disks, making them more susceptible to herniation.
- Quit smoking. Avoid the use of any tobacco products.