Overview
Stomach and pyloric valve
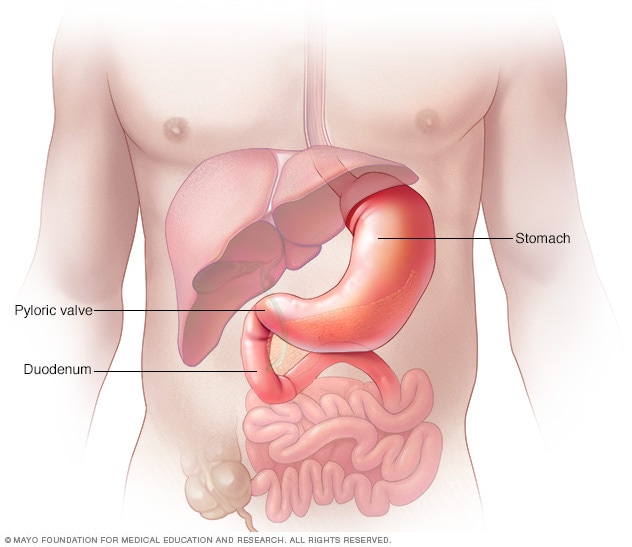
Stomach and pyloric valve
The stomach is a muscular sac. It's about the size of a small melon that expands when you eat or drink. It can hold as much as a gallon (about 4 liters) of food or liquid. Once the stomach grinds the food, strong muscle contractions called peristaltic waves push the food toward the pyloric valve. The pyloric valve leads to the upper part of the small intestine, called the duodenum.
Gastroparesis is a condition in which the muscles in the stomach don't move food as they should for it to be digested.
Most often, muscles contract to send food through the digestive tract. But with gastroparesis, the stomach's movement, called motility, slows or doesn't work at all. This keeps the stomach from emptying well.
Often, the cause of gastroparesis is not known. Sometimes it's linked to diabetes. And some people get gastroparesis after surgery or after a viral illness.
Certain medicines, such as opioid pain relievers, some antidepressants, and medicines for high blood pressure, weight loss and allergies can slow stomach emptying. The symptoms can be like those of gastroparesis. For people who already have gastroparesis, these medicines may make the condition worse.
Gastroparesis affects digestion. It can cause nausea, vomiting and belly pain. It also can cause problems with blood sugar levels and nutrition. There's no cure for gastroparesis. But medicines and changes to diet can give some relief.
Symptoms
Symptoms of gastroparesis include:
- Vomiting.
- Nausea.
- Belly bloating.
- Belly pain.
- Feeling full after eating just a few bites and long after eating a meal.
- Vomiting undigested food eaten a few hours earlier.
- Acid reflux.
- Changes in blood sugar levels.
- Not wanting to eat.
- Weight loss and not getting enough nutrients, called malnutrition.
Many people with gastroparesis don't notice any symptoms.
When to see a doctor
Make an appointment with your healthcare professional if you have symptoms that worry you.
Causes
It's not always clear what leads to gastroparesis. But sometimes damage to a nerve that controls the stomach muscles can cause it. This nerve is called the vagus nerve.
The vagus nerve helps manage what happens in the digestive tract. This includes telling the muscles in the stomach to contract and push food into the small intestine. A damaged vagus nerve can't send signals to the stomach muscles as it should. This may cause food to stay in the stomach longer.
Conditions such as diabetes or surgery to the stomach or small intestine can damage the vagus nerve and its branches.
Risk factors
Factors that can raise the risk of gastroparesis include:
- Diabetes.
- Surgery on the stomach area or on the tube that connects the throat to the stomach, called the esophagus.
- Infection with a virus.
- Certain cancers and cancer treatments, such as radiation therapy to the chest or stomach.
- Certain medicines that slow the rate of stomach emptying, such as opioid pain medicines.
- A condition that causes the skin to harden and tighten, called scleroderma.
- Nervous system diseases, such as migraine, Parkinson's disease or multiple sclerosis.
- Underactive thyroid, also called hypothyroidism.
People assigned female at birth are more likely to get gastroparesis than are people assigned male at birth.
Complications
Gastroparesis can cause several complications, such as:
- Loss of body fluids, called dehydration. Repeated vomiting can cause dehydration.
- Malnutrition. Not wanting to eat can mean you don't take in enough calories. Or your body may not be able to take in enough nutrients due to vomiting.
- Food that doesn't digest that hardens and stays in the stomach. This food can harden into a solid mass called a bezoar. Bezoars can cause nausea and vomiting. They may be life-threatening if they keep food from passing into the small intestine.
- Blood sugar changes. Gastroparesis doesn't cause diabetes. But the changes in the rate and amount of food passing into the small bowel can cause sudden changes in blood sugar levels. These blood sugar changes can make diabetes worse. In turn, poor control of blood sugar levels makes gastroparesis worse.
- Lower quality of life. Symptoms can make it hard to work and keep up with daily activities.
Sept. 06, 2024