Overview
Esophageal varices
Esophageal varices
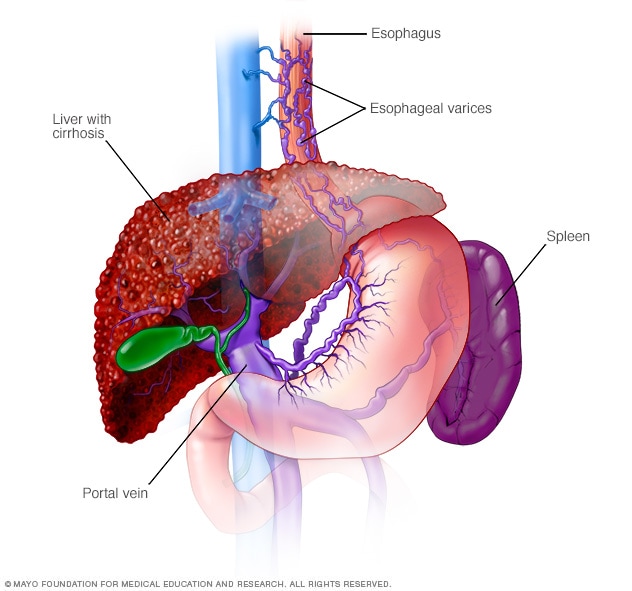
Esophageal varices are enlarged veins in the esophagus. They're often due to obstructed blood flow through the portal vein, which carries blood from the intestine to the liver.
Esophageal varices are enlarged veins in the esophagus, the tube that connects the throat and stomach. Esophageal varices most often happen in people with serious liver diseases.
Esophageal varices develop when regular blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flows into smaller blood vessels that aren't designed to carry large volumes of blood. The vessels can leak blood or even burst, causing life-threatening bleeding.
A few medicines and medical procedures are available to help prevent or stop bleeding from esophageal varices.
Symptoms
Esophageal varices usually don't cause symptoms unless they bleed. Symptoms of bleeding esophageal varices include:
- Vomiting large amounts of blood.
- Black, tarry or bloody stools.
- Lightheadedness due to blood loss.
- Loss of consciousness in severe cases.
Your doctor might suspect esophageal varices if you have signs of liver disease or been diagnosed with liver cirrhosis, including:
- Yellow coloration of the skin and eyes, known as jaundice.
- Easy bleeding or bruising.
- Fluid buildup in the abdomen, called ascites (uh-SY-teez).
When to see a doctor
Make an appointment with your health care provider if you have symptoms that worry you. If you've been diagnosed with liver disease, ask your provider about your risk of esophageal varices and what you can do to reduce your risk. Also ask whether to get a procedure to check for esophageal varices.
If you've been diagnosed with esophageal varices, your provider will likely tell you to watch for signs of bleeding. Bleeding esophageal varices are an emergency. Call 911 or your local emergency services right away if you have black or bloody stools, or bloody vomit.
Causes
Esophageal varices sometimes form when blood flow to your liver is blocked. This is most often caused by scar tissue in the liver due to liver disease, also known as cirrhosis of the liver. The blood flow begins to back up. This increases pressure within the large vein, known as the portal vein, that carries blood to your liver. This condition is called portal hypertension.
Portal hypertension forces the blood to seek other pathways through smaller veins, such as those in the lowest part of the esophagus. These thin-walled veins balloon with the added blood. Sometimes they rupture and bleed.
Causes of esophageal varices include:
- Severe liver scarring, called cirrhosis. Several liver diseases — including hepatitis infection, alcoholic liver disease, fatty liver disease and a bile duct disorder called primary biliary cholangitis — can result in cirrhosis.
- Blood clot, also called thrombosis. A blood clot in the portal vein or in a vein that feeds into the portal vein, known as the splenic vein, can cause esophageal varices.
- Parasitic infection. Schistosomiasis is a parasitic infection found in parts of Africa, South America, the Caribbean, the Middle East and East Asia. The parasite can damage the liver, as well as the lungs, intestine, bladder and other organs.
Risk factors
Although many people with advanced liver disease develop esophageal varices, most won't have bleeding. Esophageal varices are more likely to bleed if you have:
- High portal vein pressure. The risk of bleeding increases as the pressure in the portal vein increases.
- Large varices. The larger the esophageal varices, the more likely they are to bleed.
- Red marks on the varices. Some esophageal varices show long, red streaks or red spots. Your health care provider can see them through a thin, flexible tube, called an endoscope, passed down your throat. These marks suggest a high risk of bleeding.
- Severe cirrhosis or liver failure. Most often, the more severe your liver disease, the more likely esophageal varices are to bleed.
- Continued alcohol use. Your risk of variceal bleeding is far greater if you continue to drink than if you stop, especially if your disease is alcohol related.
If you've had bleeding from esophageal varices before, you're more likely to have varices that bleed again.
Complications
The most serious complication of esophageal varices is bleeding. Once you've had a bleeding episode, your risk of another bleeding episode greatly increases. If you lose enough blood, you can go into shock, which can lead to death.
Prevention
Currently, no treatment can prevent the development of esophageal varices in people with cirrhosis. While beta blocker drugs are effective in preventing bleeding in many people who have esophageal varices, they don't prevent esophageal varices from forming.
If you've been diagnosed with liver disease, ask your health care provider about strategies to avoid liver disease complications. To keep your liver healthy:
- Don't drink alcohol. People with liver disease are often advised to stop drinking alcohol, since the liver processes alcohol. Drinking alcohol may stress an already vulnerable liver.
- Eat a healthy diet. Choose a diet that's full of fruits and vegetables. Select whole grains and lean sources of protein. Reduce the amount of fatty and fried foods you eat.
- Maintain a healthy weight. An excess amount of body fat can damage your liver. Obesity is associated with a greater risk of complications of cirrhosis. Lose weight if you are obese or overweight.
- Use chemicals sparingly and carefully. Follow the directions on household chemicals, such as cleaning supplies and insect sprays. If you work around chemicals, follow all safety precautions. Your liver removes toxins from your body, so give it a break by limiting the amount of toxins it processes.
- Reduce your risk of hepatitis. Sharing needles and having unprotected sex can increase your risk of hepatitis B and C. Protect yourself by abstaining from sex or using a condom if you choose to have sex. Get tested for exposure to hepatitis A, B and C, since infection can make your liver disease worse. Also ask your health care provider whether to be vaccinated for hepatitis A and hepatitis B.