Diagnosis
To confirm a diagnosis of small bowel prolapse, your doctor performs a pelvic exam. During the exam, your doctor may ask you to take a deep breath and hold it while bearing down like you're having a bowel movement (Valsalva maneuver), which is likely to cause the prolapsed small bowel to bulge downward. If your doctor can't verify that you have a prolapse while you're lying on the exam table, he or she may repeat the exam while you're standing.
Treatment
Types of pessaries
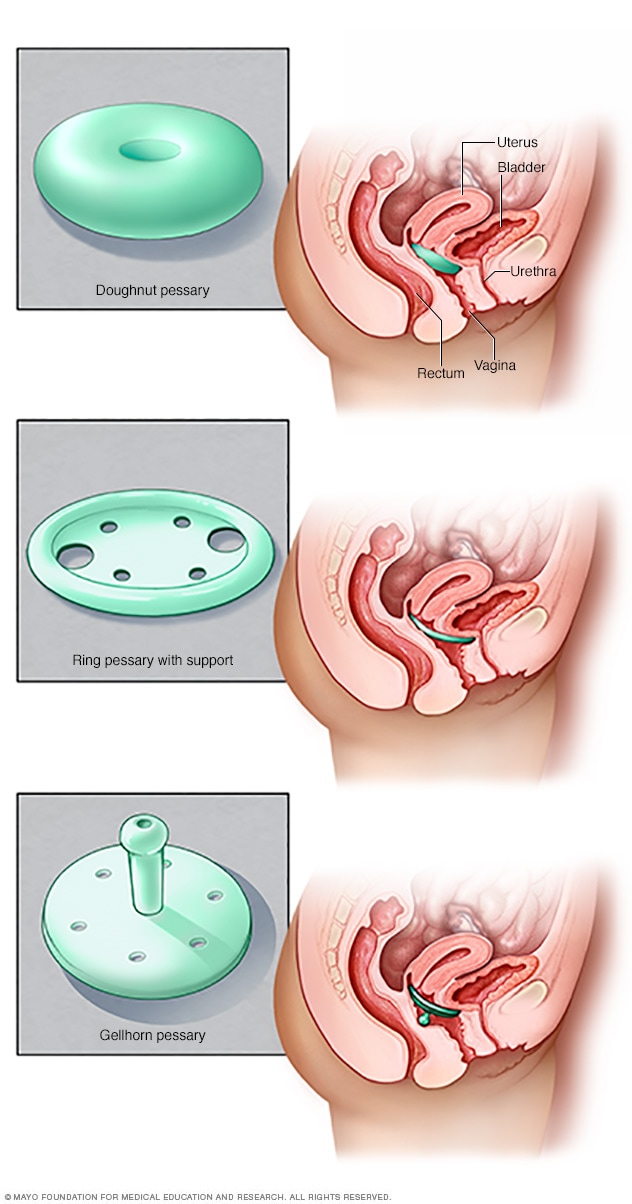
Types of pessaries
Pessaries come in many shapes and sizes. The device fits into the vagina and provides support to vaginal tissues displaced by pelvic organ prolapse. A health care provider can fit a pessary and help provide information about which type would work best.
Small bowel prolapse typically doesn't need treatment if the symptoms don't trouble you. Surgery may be effective if you have advanced prolapse with bothersome symptoms. Nonsurgical approaches are available if you wish to avoid surgery, if surgery would be too risky or if you want to become pregnant in the future.
Treatment options for small bowel prolapse include:
- Observation. If your prolapse causes few or no obvious symptoms, you don't need treatment. Simple self-care measures, such as performing exercises called Kegel exercises to strengthen your pelvic muscles, may provide symptom relief. Avoiding heavy lifting and constipation may reduce the likelihood of worsening your prolapse.
- Pessary. A silicone, plastic or rubber device inserted into your vagina supports the bulging tissue. Pessaries come in a variety of styles and sizes. Finding the right one involves some trial and error. Your doctor measures and fits you for the device, and you learn how to insert, remove and clean it.
-
Surgery. A surgeon can perform surgery to repair the prolapse through the vagina or abdomen, with or without robotic assistance. During the procedure, your surgeon moves the prolapsed small bowel back into place and tightens the connective tissue of your pelvic floor. Sometimes, small portions of synthetic mesh may be used to help support weakened tissues.
A small bowel prolapse usually doesn't recur. However, further injury to the pelvic floor can happen with increased pelvic pressure, for instance with constipation, coughing, obesity or heavy lifting.
Lifestyle and home remedies
Depending on the severity of your condition, these self-care measures may provide the symptom relief you need:
- Perform Kegel exercises to strengthen pelvic muscles and support weakened vaginal tissues.
- Avoid constipation by drinking plenty of fluids and eating high-fiber foods, such as whole grains, and fresh fruits and vegetables.
- Avoid heavy lifting.
- Try to control coughing.
- Lose weight if you're overweight or obese.
- Avoid bearing down to move your bowels. Rely on your natural colorectal function to empty your lower bowel.
- Quit smoking.
Kegel exercises
Kegel exercises strengthen your pelvic floor muscles, which, in part, support the uterus, bladder and bowel. A strong pelvic floor provides better support for your pelvic organs, prevents prolapse from worsening and relieves symptoms associated with pelvic organ prolapse.
To perform Kegel exercises, follow these steps:
- Tighten (contract) your pelvic floor muscles — the muscles you use to stop urinating.
- Hold the contraction for five seconds, then relax for five seconds. (If this is too difficult, start by holding for two seconds and relaxing for three seconds.)
- Work up to holding the contraction for 10 seconds at a time.
- Aim for at least three sets of 10 repetitions each day.
Ask your doctor for feedback on whether you're using the right muscles. Kegel exercises may be most successful when they're taught by a physical therapist and reinforced with biofeedback. Biofeedback involves using monitoring devices that help ensure you're tightening the proper muscles, with optimal intensity and length of time.
Once you've learned the proper method, you can do Kegel exercises discreetly just about anytime, whether you're sitting at your desk or relaxing on the couch.
Preparing for your appointment
Your first appointment may be with your primary care doctor or with a doctor who specializes in conditions affecting the female reproductive tract (gynecologist) or the reproductive tract and urinary system (urogynecologist, urologist).
What you can do
Here's some information to help you prepare for your appointment.
- Make a list of any symptoms you've had and for how long.
- List your key medical information, including other conditions for which you're being treated and any medications, vitamins or supplements you're taking.
- Take a family member or friend along, if possible, to help you remember all the information you'll receive.
- Write down questions to ask your doctor, listing the most important ones first in case time runs short.
For small bowel prolapse, basic questions to ask your doctor include:
- Is the prolapse causing my symptoms?
- What treatment approach do you recommend?
- What will happen if I choose not to have the prolapse treated?
- What is the risk that this problem will recur at any time in the future?
- Do I need to follow any restrictions to prevent progression?
- Are there any self-care steps I can take?
- Should I see a specialist?
Don't hesitate to ask other questions during your appointment as they occur to you.
What to expect from your doctor
Your doctor may ask questions such as:
- What symptoms do you have?
- When did you first notice these symptoms?
- Have your symptoms gotten worse over time?
- Do you have pelvic pain? If yes, how severe is the pain?
- Does anything seem to trigger your symptoms, such as coughing or heavy lifting?
- Do you have urine leakage (urinary incontinence)?
- Have you had an ongoing (chronic) or severe cough?
- Do you often lift heavy objects during work or daily activities?
- Do you strain during bowel movements?
- Do you have any other medical conditions?
- What medications, vitamins or supplements do you take?
- Have you been pregnant and had vaginal deliveries?
- Do you wish to have children in the future?
Feb. 10, 2023