Overview
Diverticulosis and diverticulitis
Diverticulosis and diverticulitis
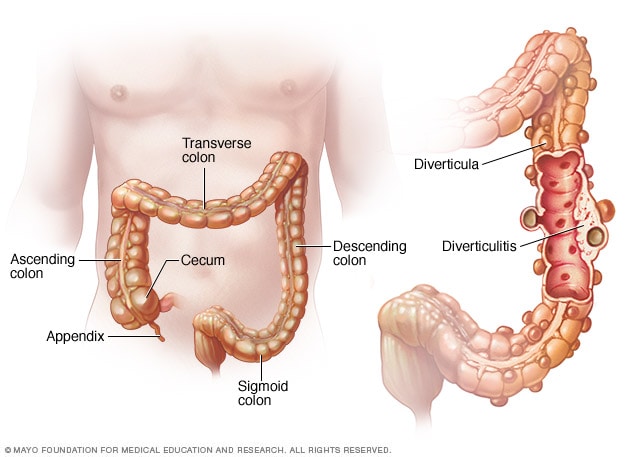
Diverticulosis occurs when small, bulging pouches (diverticula) develop in your digestive tract. When one or more of these pouches become inflamed or infected, the condition is called diverticulitis.
Diverticulitis is inflammation of irregular bulging pouches in the wall of the large intestine.
Typically, the wall of the large intestine, also called the colon, is smooth. An irregular, bulging pouch in the colon wall is called a diverticulum. Multiple pouches are called diverticula.
Diverticula are common, especially after age 50. They are usually found in the lower part of the colon. Most often, they don't cause problems. The presence of diverticula is called diverticulosis. Diverticulosis isn't a disease condition.
When these pouches become inflamed, the condition is called diverticulitis. Inflammation is immune system activity that increases blood flow and fluids to a site in the body and delivers disease-fighting cells. Inflammation of diverticula can cause severe pain, fever, nausea and changes in your stool habits.
Mild diverticulitis is usually treated with rest, changes in your diet and possibly antibiotics. Severe diverticulitis usually needs antibiotic treatment in the hospital. Surgery may be needed for severe or frequent diverticulitis.
Symptoms
A common symptom of diverticulitis is pain in the area below the chest called the abdomen. Most often, pain is in the lower left abdomen.
Pain from diverticulitis is usually sudden and intense. Pain may be mild and gradually worsen, or the intensity of the pain may vary over time.
Other signs and symptoms of diverticulitis may include:
- Nausea.
- Fever.
- Tenderness in the abdomen when touched.
- Changes in stool, including sudden diarrhea or constipation.
When to see a doctor
Get medical care anytime you have constant, unexplained abdominal pain, particularly if you also have a fever and notable changes in stools.
Causes
Diverticula gradually develop over time in the walls of the colon. They are common in older adults. Pressure in the colon — possibly from spasms or straining — may cause diverticula to form where the wall of the colon is weak.
Diverticulitis is inflammation of one or more diverticula. This may happen because of bacterial disease or damage to diverticula tissues.
Risk factors
Diverticulitis is more common among people over 50. Other factors that increase the risk of diverticulitis include:
- Obesity.
- Smoking.
- A diet of low-fiber foods.
- A diet high in red meat.
- Heavy alcohol use.
- Lack of exercise.
- Low vitamin D levels.
- Certain medicines, such as steroids, opioids and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
Complications
About 15 percent of people with diverticulitis develop complications. These may include:
- A pocket of pus from bacterial disease, called an abscess.
- Blockage of the colon.
- An irregular passageway, called a fistula, between the bowel and another organ in the body.
- A tear in the colon wall that allows waste to spill out, causing serious disease of the abdomen lining, called peritonitis.
- Bleeding from ruptured blood vessels, also called diverticular hemorrhage.
Prevention
To help prevent diverticulitis:
- Exercise regularly. Regular, vigorous exercise decreases the risk of diverticulitis.
- Eat a high-fiber diet. A high-fiber diet improves the movement of waste through the colon and decreases the risk of diverticulitis. Fiber-rich foods include fruits, vegetables, whole grains, seeds and beans. Cut back on red meats and sweets.
- Maintain a healthy weight. Talk to your healthcare professional or a dietitian about goals for a healthy weight for you and strategies to reach your goals.
- Drink plenty of fluids. Fiber works by absorbing water and increasing the soft, bulky waste in your colon. Drinking fluids improves the movement of waste and prevents constipation.
- Quit smoking and limit alcohol use. Smoking and heavy alcohol use are associated with an increased risk of diverticulitis.
In the past, healthcare professionals recommended that people with diverticulitis avoid nuts, seeds and popcorn. Studies have shown that these foods do not increase the risk of diverticulitis. Seeds and some nuts are good sources of fiber.
Oct. 22, 2024