Overview
Cranial sutures and fontanels
Cranial sutures and fontanels
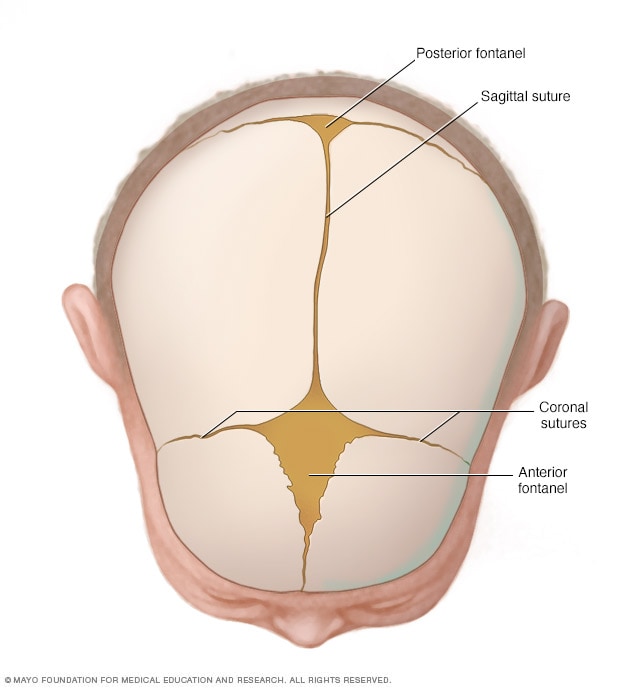
Joints called cranial sutures are made of flexible, fibrous tissue. They hold the bones of a baby's skull together. The sutures meet at the fontanels, the soft spots on a baby's head. The sutures remain flexible during infancy. This allows the skull to grow as the brain grows. The largest fontanel, called the anterior fontanel, is at the front.
Craniosynostosis (kray-nee-o-sin-os-TOE-sis) is a condition present at birth. It causes one or more of the joints between the bones of a baby's skull to close too early, before the brain is fully formed.
A baby's skull is made up of small plates of bone connected by flexible, fibrous joints called sutures. The sutures allow a baby's skull to get bigger as the brain grows. The sutures usually close when the brain is done growing.
Craniosynostosis usually involves early closing of one cranial suture but can involve more than one. Brain growth continues even when one or more sutures close too early. Open sutures on other sides of the head allow brain growth in those directions. This causes the head to have a shape that's not typical.
Treating craniosynostosis involves surgery to reshape the skull. Early diagnosis and treatment allow the baby's brain enough space to grow and develop.
After surgery, most children develop as expected and have a more average shape to the face and head.
Products & Services
Symptoms
Symptoms of craniosynostosis usually can be seen at birth. They become easier to see during the first few months of a baby's life.
Symptoms and their severity depend on how many sutures are closed and when the closing occurs during brain development. Symptoms can include:
- A skull with a shape that's not typical. Shape depends on which of the sutures are closed. The brain keeps growing on the sides with open sutures, changing the shape of the head.
- Change in the balance of facial features and ears. For example, one eye may be higher than the other.
- A raised, hard ridge along the closed cranial suture.
Types of craniosynostosis
On the top of the head toward the front, some sutures meet at the large soft spot called the anterior fontanel. The anterior fontanel is the soft spot felt just behind a baby's forehead. The next largest fontanel, called the posterior fontanel, is at the back of the head where the other sutures meet. The flexible, fibrous sutures connect the bony plates of the skull.
The term given to each type of craniosynostosis depends on which sutures are affected. Types of craniosynostosis include:
- Sagittal. The sagittal suture runs from front to back at the top of the skull between the front and back fontanels. When the sagittal suture closes too early, it forces the head to grow long and narrow. Sagittal craniosynostosis is the most common type of craniosynostosis.
- Coronal. Coronal sutures run from each ear to the top of the skull, meeting at the front fontanel. When only one coronal suture closes too early, it may cause the forehead to flatten on that side and bulge on the other side. It also causes the nose to turn and the eye socket to rise on the affected side. When both coronal sutures close too early, the head looks short and wide, often with the forehead tilted forward.
- Metopic. The metopic suture runs up from the top of the bridge of the nose through the middle of the forehead to the front fontanel. When the metopic suture closes too early, the forehead has a triangular shape and the back part of the head widens.
- Lambdoid. The lambdoid suture runs down the back of the head from the back fontanel. When the lambdoid suture closes too early, it may cause one side of a baby's head to appear flat, one ear to be higher than the other ear and the top of the head to tilt to one side. Early closing of the lambdoid suture is a very rare type of craniosynostosis.
Other reasons for a changed head shape
A head shape that's not typical doesn't always mean that a baby has craniosynostosis. For example, if the back of your baby's head appears flattened, it could be the result of spending too much time lying on the back. This can be treated with regular position changes. If the head is very flat on one side, helmet therapy can help reshape the head to a more balanced look.
When to see a doctor
Your pediatrician or other healthcare professional monitors your child's head growth at well-child visits. Talk with your healthcare professional if you have concerns about your baby's head growth or shape.
Causes
Often the cause of craniosynostosis is not known. But sometimes it's related to genetic conditions.
- Nonsyndromic craniosynostosis is the most common type. Its cause is not known, but it's thought to be a mix of genetic and environmental factors.
- Syndromic craniosynostosis is caused by certain gene changes that cause genetic syndromes. Examples include Apert syndrome, Pfeiffer syndrome and Crouzon syndrome. These syndromes can affect a baby's skull development. They usually also include other physical changes and health conditions.
Risk factors
Genetic syndromes that affect a baby's skull development, such as Apert syndrome, Pfeiffer syndrome and Crouzon syndrome, are risk factors for craniosynostosis.
Complications
If not treated, craniosynostosis may cause:
- Lasting changes in the shape of the head and face.
- A feeling of not being worthy and of wanting to stay away from others.
The risk of higher pressure inside the skull, called intracranial pressure, from craniosynostosis is small if the suture and head shape are treated with surgery. Babies who have craniosynostosis caused by a genetic syndrome may develop higher pressure inside the skull if treatment doesn't make the skull larger to make room for their growing brains.
If not treated, higher pressure inside the skull can cause:
- Developmental delays.
- Problems with thinking, memory and learning.
- Blindness.
- Seizures.
- Headaches.
Aug. 01, 2025