Overview
Congenital heart disease is one or more problems with the heart's structure that are present at birth. Congenital means that you're born with the condition. A congenital heart condition can change the way blood flows through the heart.
There are many different types of congenital heart defects. This article focuses on congenital heart disease in adults.
Some types of congenital heart disease may be mild. Others may cause life-threatening complications. Advances in diagnosis and treatment have improved survival for those born with a heart problem.
Treatment for congenital heart disease may include regular health checkups, medicines or surgery. If you have adult congenital heart disease, ask your healthcare professional how often you need a checkup.
Products & Services
Types
Symptoms
Some people born with a heart problem don't notice symptoms until later in life. Symptoms also may return years after a congenital heart defect is treated.
Common congenital heart disease symptoms in adults include:
- Irregular heartbeats, called arrhythmias.
- Blue or gray skin, lips and fingernails due to low oxygen levels. Depending on the skin color, these changes may be harder or easier to see.
- Shortness of breath.
- Feeling tired very quickly with activity.
- Swelling due to fluid collecting inside body tissues, called edema.
When to see a doctor
Get emergency medical help if you have unexplained chest pain or shortness of breath.
Make an appointment for a health checkup if:
- You have symptoms of adult congenital heart disease.
- You received treatment for a congenital heart defect as a child.
Causes
Chambers and valves of the heart
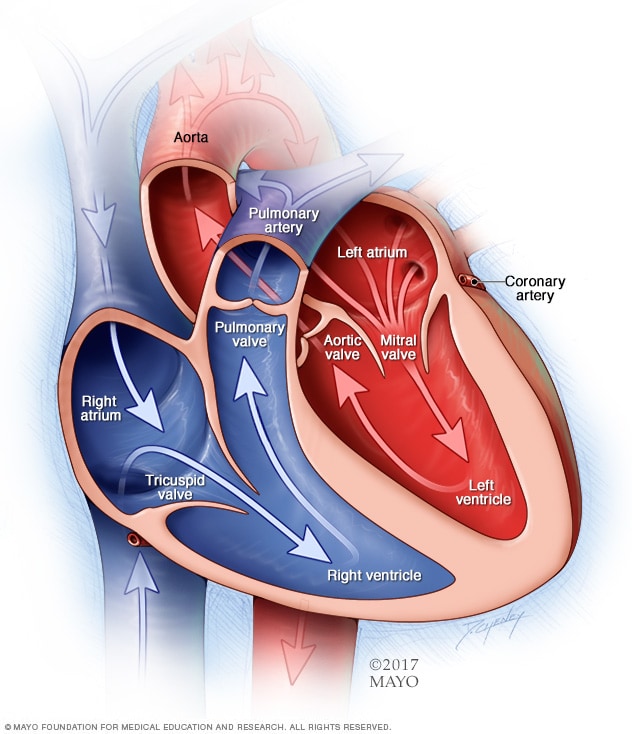
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
Researchers aren't sure what causes most types of congenital heart disease. They think that gene changes, certain medicines or health conditions, and environmental or lifestyle factors, such as smoking, may play a role.
Risk factors
Risk factors for congenital heart disease include:
- Genetics. Congenital heart disease appears to run in families, which means it is inherited. Changes in genes have been linked to heart problems present at birth. For instance, people with Down syndrome are often born with heart conditions.
- German measles, also called rubella. Having rubella during pregnancy may affect how the baby's heart grows while in the womb. A blood test done before pregnancy can find out if you're immune to rubella. A vaccine is available for those who aren't immune.
- Diabetes. Having type 1 or type 2 diabetes during pregnancy also may change how the baby's heart grows while in the womb. Gestational diabetes generally doesn't increase the risk of congenital heart disease.
- Medicines. Taking certain medicines during pregnancy can cause congenital heart disease and other health problems present at birth. Medicines linked to congenital heart defects include lithium (Lithobid) for bipolar disorder and isotretinoin (Claravis, Myorisan, others), which is used to treat acne. Always tell your healthcare team about the medicines you take.
- Alcohol. Drinking alcohol while pregnant has been linked to heart conditions in the baby.
- Smoking. If you smoke, quit. Smoking during pregnancy increases the risk of congenital heart defects in the baby.
Complications
Complications of congenital heart disease may occur years after the heart condition is treated.
Complications of congenital heart disease in adults include:
- Irregular heartbeats, called arrhythmias. Scar tissue in the heart from surgeries to fix a congenital heart condition can lead to changes in heart signaling. The changes can cause the heart to beat too fast, too slow or irregularly. Some irregular heartbeats may cause stroke or sudden cardiac death if not treated.
- Infection of the lining of the heart and heart valves, called endocarditis. Untreated, this infection can damage or destroy the heart valves or cause a stroke. Antibiotics may be recommended before dental care to prevent this infection. Regular dental checkups are important. Healthy gums and teeth reduce the risk of endocarditis.
- Stroke. Congenital heart disease can let a blood clot pass through the heart and travel to the brain, causing a stroke.
- High blood pressure in the lung arteries, called pulmonary hypertension. Some heart conditions present at birth send more blood to the lungs, causing pressure to build. This eventually causes the heart muscle to weaken and sometimes to fail.
- Heart failure. The heart can't pump enough blood to meet the body's needs.
Adult congenital heart disease and pregnancy
It may be possible to have a successful pregnancy with mild congenital heart disease. A healthcare professional may tell you not to get pregnant if you have complex congenital heart disease.
Before becoming pregnant, talk with your healthcare team about the possible risks and complications. Together you can discuss and plan for any special care needed during pregnancy.
Prevention
Because the exact cause of most congenital heart disease is unknown, it may not be possible to prevent these heart conditions. Some types of congenital heart disease occur in families. If you have a high risk of giving birth to a child with a congenital heart defect, genetic testing and screening may be done during pregnancy.