Overview
Cardiomyopathy (kahr-dee-o-my-OP-uh-thee) is a disease of the heart muscle. It causes the heart to have a harder time pumping blood to the rest of the body, which can lead to symptoms of heart failure. Cardiomyopathy also can lead to some other serious heart conditions.
There are various types of cardiomyopathy. The main types include dilated, hypertrophic and restrictive cardiomyopathy. Treatment includes medicines and sometimes surgically implanted devices and heart surgery. Some people with severe cardiomyopathy need a heart transplant. Treatment depends on the type of cardiomyopathy and how serious it is.
Types
Symptoms
Some people with cardiomyopathy don't ever get symptoms. For others, symptoms appear as the condition becomes worse. Cardiomyopathy symptoms can include:
- Shortness of breath or trouble breathing with activity or even at rest.
- Chest pain, especially after physical activity or heavy meals.
- Heartbeats that feel rapid, pounding or fluttering.
- Swelling of the legs, ankles, feet, stomach area and neck veins.
- Bloating of the stomach area due to fluid buildup.
- Cough while lying down.
- Trouble lying flat to sleep.
- Fatigue, even after getting rest.
- Dizziness.
- Fainting.
Symptoms tend to get worse unless they are treated. In some people, the condition becomes worse quickly. In others, it might not become worse for a long time.
When to see a doctor
See your healthcare professional if you have any symptoms of cardiomyopathy. Call 911 or your local emergency number if you faint, have trouble breathing or have chest pain that lasts for more than a few minutes.
Some types of cardiomyopathy can be passed down through families. If you have the condition, your healthcare professional might recommend that your family members be checked.
Causes
Dilated cardiomyopathy

Dilated cardiomyopathy
Dilated cardiomyopathy causes the chambers of the heart to grow larger. Untreated, dilated cardiomyopathy can lead to heart failure.
Hypertrophic cardiomyopathy
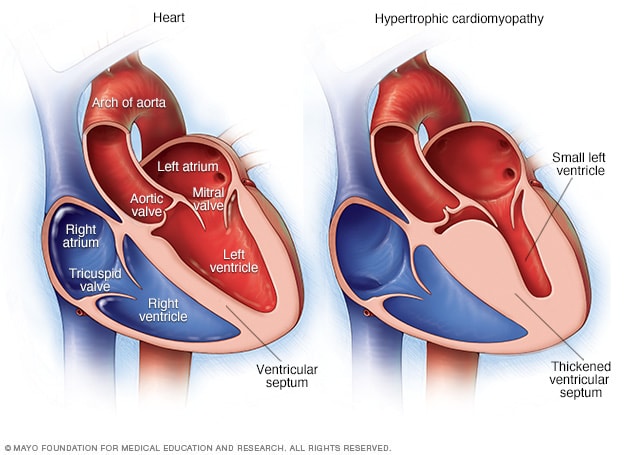
Hypertrophic cardiomyopathy
Illustrations of a typical heart, as shown on the left, and a heart with hypertrophic cardiomyopathy. Note that the heart walls are much thicker in the heart with hypertrophic cardiomyopathy.
Often, the cause of the cardiomyopathy isn't known. But some people get it due to another condition. This is known as acquired cardiomyopathy. Other people are born with cardiomyopathy because of a gene passed on from a parent. This is called inherited cardiomyopathy.
Certain health conditions or behaviors that can lead to acquired cardiomyopathy include:
- Long-term high blood pressure.
- Heart tissue damage from a heart attack.
- Long-term rapid heart rate.
- Heart valve problems.
- COVID-19 infection.
- Certain infections, especially those that cause inflammation of the heart.
- Metabolic disorders, such as obesity, thyroid disease or diabetes.
- Lack of essential vitamins or minerals in the diet, such as thiamin (vitamin B-1).
- Pregnancy complications.
- Iron buildup in the heart muscle, called hemochromatosis.
- The growth of tiny lumps of inflammatory cells called granulomas in any part of the body. When this happens in the heart or lungs, it's called sarcoidosis.
- The buildup of irregular proteins in the organs, called amyloidosis.
- Connective tissue disorders.
- Drinking too much alcohol over many years.
- Use of cocaine, amphetamines or anabolic steroids.
- Use of some chemotherapy medicines and radiation to treat cancer.
Types of cardiomyopathy include:
-
Dilated cardiomyopathy. In this type of cardiomyopathy, the heart's chambers thin and stretch, growing larger. The condition tends to start in the heart's main pumping chamber, called the left ventricle. As a result, the heart has trouble pumping blood to the rest of the body.
This type can affect people of all ages. But it happens most often in people younger than 50 and is more likely to affect men. Conditions that can lead to a dilated heart include coronary artery disease and heart attack. But for some people, gene changes play a role in the disease.
-
Hypertrophic cardiomyopathy. In this type, the heart muscle becomes thickened. This makes it harder for the heart to work. The condition mostly affects the muscle of the heart's main pumping chamber.
Hypertrophic cardiomyopathy can start at any age. But it tends to be worse if it happens during childhood. Most people with this type of cardiomyopathy have a family history of the disease. Some gene changes have been linked to hypertrophic cardiomyopathy. The condition doesn't happen due to a heart problem.
-
Restrictive cardiomyopathy. In this type, the heart muscle becomes stiff and less flexible. As a result, it can't expand and fill with blood between heartbeats. This least common type of cardiomyopathy can happen at any age. But it most often affects older people.
Restrictive cardiomyopathy can occur for no known reason, also called an idiopathic cause. Or it can by caused by a disease elsewhere in the body that affects the heart, such as amyloidosis.
- Arrhythmogenic right ventricular cardiomyopathy (ARVC). This is a rare type of cardiomyopathy that tends to happen between the ages of 10 and 50. It mainly affects the muscle in the lower right heart chamber, called the right ventricle. The muscle is replaced by fat that can become scarred. This can lead to heart rhythm problems. Sometimes, the condition involves the left ventricle as well. ARVC often is caused by gene changes.
- Unclassified cardiomyopathy. Other types of cardiomyopathy fall into this group.
Risk factors
Many things can raise the risk of cardiomyopathy, including:
- Family history of cardiomyopathy, heart failure and sudden cardiac arrest.
- Long-term high blood pressure.
- Conditions that affect the heart. These include a past heart attack, coronary artery disease or an infection in the heart.
- Obesity, which makes the heart work harder.
- Long-term alcohol misuse.
- Illicit drug use, such as cocaine, amphetamines and anabolic steroids.
- Treatment with certain chemotherapy medicines and radiation for cancer.
Many diseases also raise the risk of cardiomyopathy, including:
- Diabetes.
- Thyroid disease.
- Storage of excess iron in the body, called hemochromatosis.
- Buildup of a certain protein in organs, called amyloidosis.
- The growth of small patches of inflamed tissue in organs, called sarcoidosis.
- Connective tissue disorders.
Complications
Enlarged heart, in heart failure
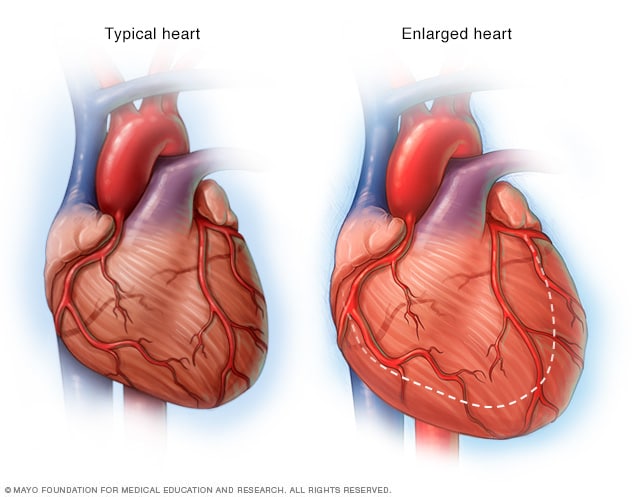
Enlarged heart, in heart failure
If the heart weakens, as it can with heart failure, it begins to enlarge. This forces the heart to work harder to pump blood to the rest of the body.
Cardiomyopathy can lead to serious medical conditions, including:
- Heart failure. The heart can't pump enough blood to meet the body's needs. Without treatment, heart failure can be life-threatening.
- Blood clots. Because the heart can't pump well, blood clots might form in the heart. If clots enter the bloodstream, they can block the blood flow to other organs, including the heart and brain.
- Heart valve problems. Because cardiomyopathy can cause the heart to become larger, the heart valves might not close properly. This can cause blood to flow backward in the valve.
- Cardiac arrest and sudden death. Cardiomyopathy can trigger irregular heart rhythms that cause fainting. Sometimes, irregular heartbeats can cause sudden death if the heart stops beating effectively.
Prevention
Inherited types of cardiomyopathy can't be prevented. Let your healthcare professional know if you have a family history of the condition.
You can help lower the risk of acquired types of cardiomyopathy, which are caused by other conditions. Take steps to lead a heart-healthy lifestyle, including:
- Stay away from alcohol or illegal drugs such as cocaine.
- Control any other conditions you have, such as high blood pressure, high cholesterol or diabetes.
- Eat a healthy diet.
- Get regular exercise.
- Get enough sleep.
- Lower your stress.
These healthy habits also can help people with inherited cardiomyopathy control their symptoms.
Feb. 21, 2024