Diagnosis
To diagnose your condition, your healthcare professional checks your symptoms and does a physical exam. To know how serious your brachial plexus injury is, you may need one or more of the following tests:
- X-ray. An X-ray of the shoulder and neck can show fractures or other related injuries.
- Electromyography (EMG). During an EMG, a healthcare professional places a needle electrode through the skin into different muscles. The test looks at the electrical activity of the muscles when they tighten and when they're at rest. You may feel a little pain when the electrodes are put in, but most people can finish the test without much discomfort.
- Nerve conduction studies. These tests are usually done as part of EMG. They measure how fast and how well electrical signals travel down the nerves. This provides information about how well the nerve is working.
- Magnetic resonance imaging (MRI). This test uses a powerful magnetic field and radio waves to make very detailed images of the organs and tissues in the body. It can show how much damage there is to the brachial plexus after an injury. It also can show any artery damage in the limb, which is important for reconstruction. New types of high-resolution MRI, such as magnetic resonance neurography or diffusion tensor imaging, may be used.
- Computerized tomography (CT) myelography. Computerized tomography uses a series of X-rays to create images of the body. CT myelography uses contrast dye, injected during a spinal tap, to look for issues in the spinal cord and nerve roots. This test is sometimes done when MRIs don't give enough information.
More Information
Treatment
Treatment depends on many factors, such as the seriousness of the injury, the type of injury, the length of time since the injury and other existing conditions.
Nerves that have only been stretched may heal on their own.
Your healthcare team may suggest physical therapy to keep the joints and muscles working properly, maintain range of motion, and prevent stiff joints.
Surgery is often the best option for serious nerve injuries. In the past, surgery was sometimes delayed to see if the nerves would heal on their own. However, new research shows that delaying surgery by more than 2 to 6 months could make the repair less successful. New imaging techniques can help your healthcare team decide when surgery would be most beneficial.
Nerve tissue grows slowly, so it can take many years before you see the final results of surgery. During recovery, you can do exercises to keep your joints flexible. Splints may be used to keep the hand from curling inward.
Types of surgery
Nerve graft
Nerve graft
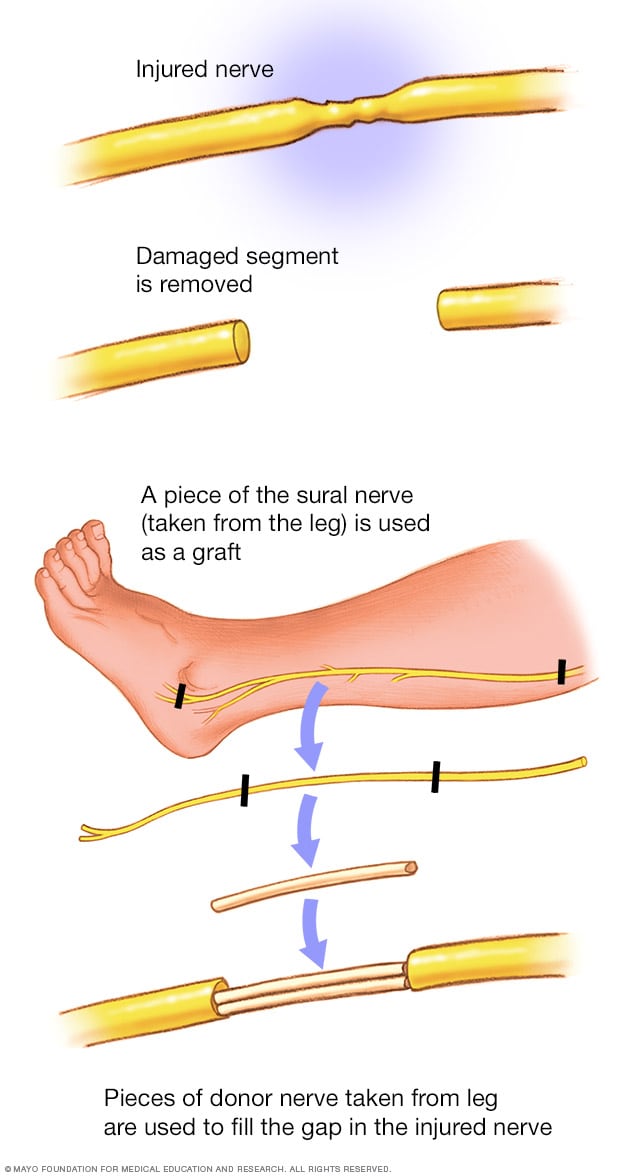
Nerve tissue can be taken from other parts of the body to replace the damaged parts of the brachial plexus nerves.
Nerve transfer

Nerve transfer
Nerve transfers are most helpful for serious brachial plexus injuries, called avulsions. An avulsion happens when the nerve root has been torn out of the spinal cord. Nerve transfers also may be used to speed up muscle recovery. Because the nerve reconstruction is often close to the muscle, nerve recovery may be faster and better than it is with other techniques.
Muscle transfer
Muscle transfer
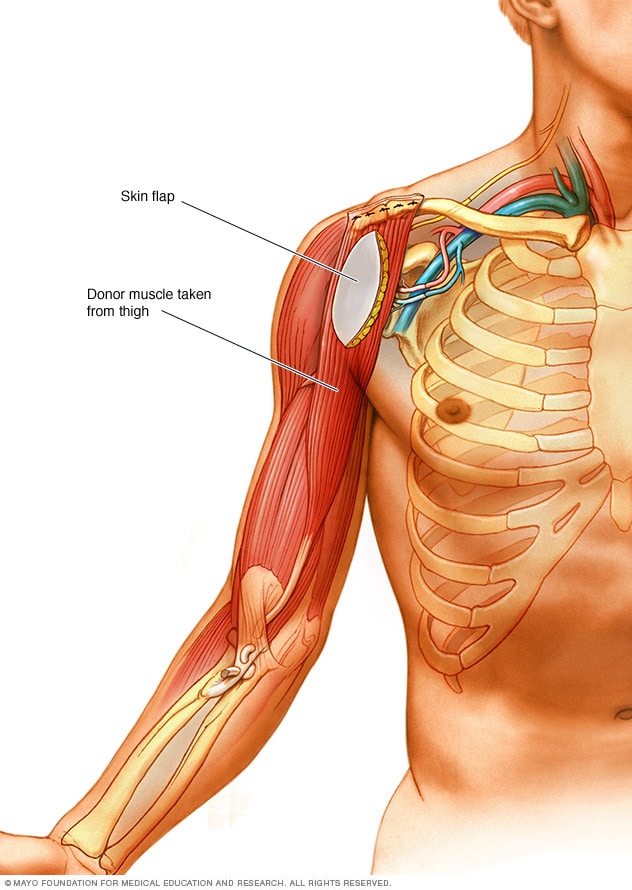
If the arm muscles are weak from lack of use, a muscle transfer may be needed. The most used donor muscle is in the inner thigh. A section of skin and tissue attached to the donor muscle may also be removed. This skin flap can help the surgeons check whether the muscle is getting enough blood after it has been transferred to its new location.
- Neurolysis. This procedure is used to free up the nerves from scar tissue.
- Nerve repair. This involves directly repairing nerves injured by sharp objects, such as knives. Rarely, this can be done when nerve fibers are stretched.
- Nerve graft. A nerve graft uses nerves from other parts of the body to replace the damaged part of the brachial plexus. This creates a bridge for new nerve growth over time.
- Nerve transfer. When the nerve root has been torn from the spinal cord, surgeons often take a less important nerve that's still working and connect it to a nerve that's more important but not working. This allows for new nerve growth.
- Muscle transfer. In muscle transfer, a surgeon removes a less important muscle or tendon from another part of the body, such as the thigh, transfers it to the arm, and reconnects the nerves and blood vessels to the muscle.
Pain control
Serious brachial plexus injuries can cause extreme pain. The pain has been described as a debilitating, severe, crushing feeling or a constant burning. This pain goes away within three years for most people. If medicine can't control the pain, your healthcare team might suggest surgery to interrupt the pain signals coming from the damaged part of the spinal cord.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Preparing for your appointment
Many tests may be used to help diagnose brachial plexus injuries. When you make your appointment, be sure to ask whether you need to prepare for these tests. For example, you may need to stop taking certain medicines for a few days or avoid using lotions the day of the test.
If possible, bring a family member or friend. Sometimes it can be hard to remember all the information you're given during an appointment. Someone who goes with you may remember something that you forgot or missed.
Other tips for getting the most from your appointment are:
- Write down all your symptoms, including how you were injured, how long you've had your symptoms and whether they've gotten worse over time.
- Make a list of all medicines, vitamins and supplements that you're taking.
- Don't hesitate to ask questions. Children and adults with brachial plexus injuries have many options for restoring movement. Be sure to ask your healthcare team about all the possibilities available to you or your child. If you run out of time, ask to speak with a nurse or have a member of your care team call you later.