Diagnosis
Endoscopy is generally used to determine if you have Barrett's esophagus.
A lighted tube with a camera at the end (endoscope) is passed down your throat to check for signs of changing esophagus tissue. Normal esophagus tissue appears pale and glossy. In Barrett's esophagus, the tissue appears red and velvety.
Your doctor will remove tissue (biopsy) from your esophagus. The biopsied tissue can be examined to determine the degree of change.
Determining the degree of tissue change
A doctor who specializes in examining tissue in a laboratory (pathologist) determines the degree of dysplasia in your esophagus cells. Because it can be difficult to diagnose dysplasia in the esophagus, it's best to have two pathologists — with at least one who specializes in gastroenterology pathology — agree on your diagnosis. Your tissue may be classified as:
- No dysplasia, if Barrett's esophagus is present but no precancerous changes are found in the cells.
- Low-grade dysplasia, if cells show small signs of precancerous changes.
- High-grade dysplasia, if cells show many changes. High-grade dysplasia is thought to be the final step before cells change into esophageal cancer.
Screening for Barrett's esophagus
Barrett's esophagus diagnosis

Barrett's esophagus diagnosis
Barrett's esophagus has a distinct appearance when viewed during an endoscopy exam. During endoscopy, the doctor passes a flexible tube with a video camera at the tip (endoscope) down your throat and into the swallowing tube (your esophagus). The video camera detects surface abnormalities, such as acid reflux damage or the presence of a hiatal hernia or ulcers, as well as Barrett's esophagus.
The American College of Gastroenterology says screening may be recommended for men who have had GERD symptoms at least weekly that don't respond to treatment with proton pump inhibitor medication, and who have at least two more risk factors, including:
- Having a family history of Barrett's esophagus or esophageal cancer
- Being male
- Being white
- Being over 50
- Being a current or past smoker
- Having a lot of abdominal fat
While women are significantly less likely to have Barrett's esophagus, women should be screened if they have uncontrolled reflux or have other risk factors for Barrett's esophagus.
Treatment
Treatment for Barrett's esophagus depends on the extent of abnormal cell growth in your esophagus and your overall health.
No dysplasia
Your doctor will likely recommend:
- Periodic endoscopy to monitor the cells in your esophagus. If your biopsies show no dysplasia, you'll probably have a follow-up endoscopy in one year and then every three to five years if no changes occur.
- Treatment for GERD. Medication and lifestyle changes can ease your signs and symptoms. Surgery or endoscopy procedures to correct a hiatal hernia or to tighten the lower esophageal sphincter that controls the flow of stomach acid may be an option.
Low-grade dysplasia
Low-grade dysplasia is considered the early stage of precancerous changes. If low-grade dysplasia is found, it should be verified by an experienced pathologist. For low-grade dysplasia, your doctor may recommend another endoscopy in six months, with additional follow-up every six to 12 months.
But, given the risk of esophageal cancer, treatment may be recommended if the diagnosis is confirmed. Preferred treatments include:
- Endoscopic resection, which uses an endoscope to remove damaged cells to aid in the detection of dysplasia and cancer.
- Radiofrequency ablation, which uses heat to remove abnormal esophagus tissue. Radiofrequency ablation may be recommended after endoscopic resection.
- Cryotherapy, which uses an endoscope to apply a cold liquid or gas to abnormal cells in the esophagus. The cells are allowed to warm up and then are frozen again. The cycle of freezing and thawing damages the abnormal cells.
If significant inflammation of the esophagus is present at initial endoscopy, another endoscopy is performed after you've received three to four months of treatment to reduce stomach acid.
High-grade dysplasia
GERD surgery
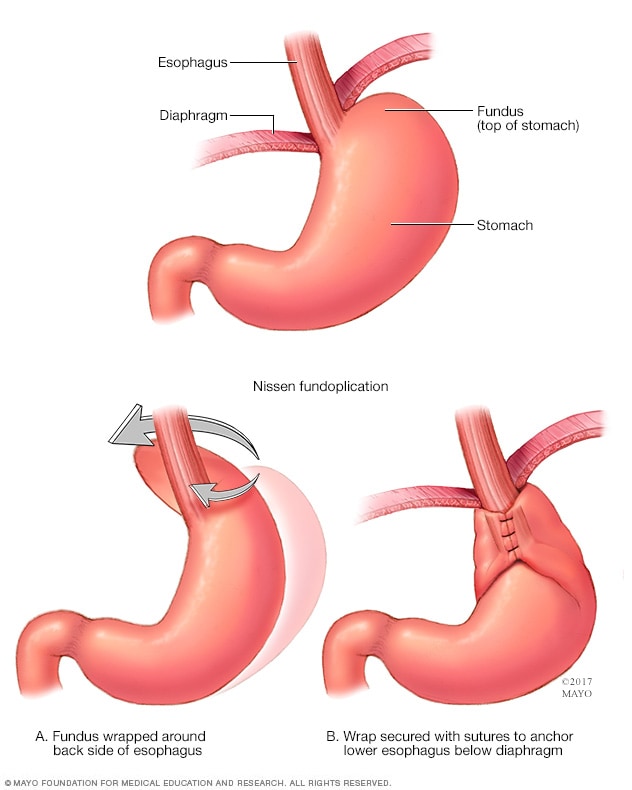
GERD surgery
Surgery for GERD may involve a procedure to reinforce the lower esophageal sphincter. The procedure is called Nissen fundoplication. In this procedure, the surgeon wraps the top of the stomach around the lower esophagus. This reinforces the lower esophageal sphincter, making it less likely that acid will back up in the esophagus.
High-grade dysplasia is generally thought to be a precursor to esophageal cancer. For this reason, your doctor may recommend endoscopic resection, radiofrequency ablation or cryotherapy. Another option may be surgery, which involves removing the damaged part of your esophagus and attaching the remaining portion to your stomach.
Recurrence of Barrett's esophagus is possible after treatment. Ask your doctor how often you need to come back for follow-up testing. If you have treatment other than surgery to remove abnormal esophageal tissue, your doctor is likely to recommend lifelong medication to reduce acid and help your esophagus heal.
More Information
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Lifestyle changes can ease symptoms of GERD, which may underlie Barrett's esophagus. Consider:
- Maintaining a healthy weight.
- Eliminating foods and drinks that trigger your heartburn, such as chocolate, coffee, alcohol and mint.
- Stopping smoking.
- Raising the head of your bed. Place wooden blocks under your bed to elevate your head.
Preparing for your appointment
Barrett's esophagus is most often diagnosed in people with GERD who are being examined for GERD complications. If your doctor discovers Barrett's esophagus on an endoscopy exam, you may be referred to a doctor who treats digestive diseases (gastroenterologist).
What you can do
- Be aware of any pre-appointment restrictions, such as not eating solid food on the day before your appointment.
- Write down your symptoms, including any that may seem unrelated to the reason why you scheduled the appointment.
- Make a list of all your medications, vitamins and supplements.
- Write down your key medical information, including other conditions.
- Ask a relative or friend to accompany you to help you remember what the doctor says.
- Write down questions to ask your doctor.
Questions to ask your doctor
- Do my lab reports show precancerous changes (dysplasia)? If so, what is the grade of my dysplasia?
- How much of my esophagus is affected?
- How often should I be screened for changes to my esophagus?
- Do I have dysplasia and if so was it confirmed by an expert pathologist?
- What's my risk of esophageal cancer?
- What are the treatment options?
- Do I need to make diet or other lifestyle changes?
- I have other health conditions. How can I best manage these conditions together?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask additional questions during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may make time to go over points you want to spend more time on. You may be asked:
- When did you first begin experiencing symptoms? How severe are they?
- Are your symptoms continuous or occasional?
- What, if anything, seems to worsen your symptoms? Does anything make your symptoms better?
- Do you experience acid reflux symptoms?
- Do you take any medications for reflux or indigestion?
- Do you have difficulty swallowing?
- Have you lost weight?
Feb. 08, 2023