Overview
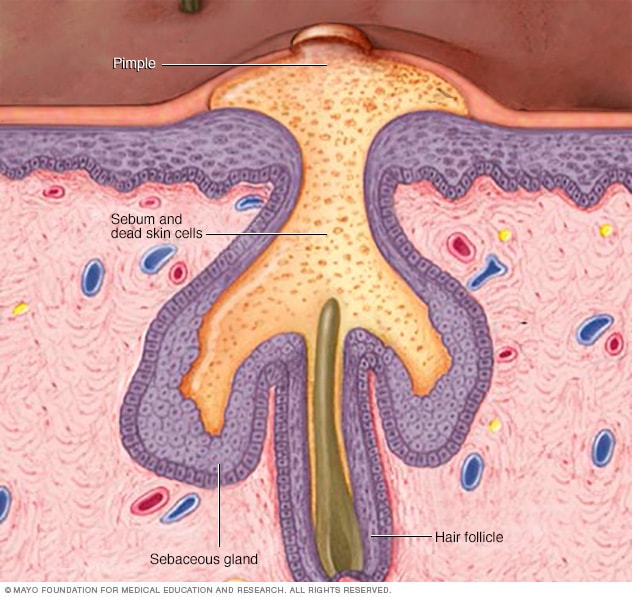
Acne is a skin condition that occurs when your hair follicles become plugged with oil and dead skin cells. It causes whiteheads, blackheads or pimples. Acne is most common among teenagers, though it affects people of all ages.
Effective acne treatments are available, but acne can be persistent. The pimples and bumps heal slowly, and when one begins to go away, others seem to crop up.
Depending on its severity, acne can cause emotional distress and scar the skin. The earlier you start treatment, the lower your risk of such problems.
Products & Services
Symptoms
Cystic acne

Cystic acne
Cystic acne — the most severe form of acne — occurs when oil and dead skin cells build up deep within hair follicles. The resulting rupture within your skin may form boil-like inflammation.
Acne signs vary depending on the severity of your condition:
- Whiteheads (closed plugged pores)
- Blackheads (open plugged pores)
- Small red, tender bumps (papules)
- Pimples (pustules), which are papules with pus at their tips
- Large, solid, painful lumps under the skin (nodules)
- Painful, pus-filled lumps under the skin (cystic lesions)
Acne usually appears on the face, forehead, chest, upper back and shoulders.
When to see a doctor
If self-care remedies don't clear your acne, see your primary care doctor. He or she can prescribe stronger medications. If acne persists or is severe, you may want to seek medical treatment from a doctor who specializes in the skin (dermatologist or pediatric dermatologist).
For many women, acne can persist for decades, with flares common a week before menstruation. This type of acne tends to clear up without treatment in women who use contraceptives.
In older adults, a sudden onset of severe acne may signal an underlying disease requiring medical attention.
The Food and Drug Administration (FDA) warns that some popular nonprescription acne lotions, cleansers and other skin products can cause a serious reaction. This type of reaction is quite rare, so don't confuse it with any redness, irritation or itchiness that occurs in areas where you've applied medications or products.
Seek emergency medical help if after using a skin product you experience:
- Faintness
- Difficulty breathing
- Swelling of the eyes, face, lips or tongue
- Tightness of the throat
Causes
How acne develops
How acne develops
Acne develops when sebum — an oily substance that lubricates your hair and skin — and dead skin cells plug hair follicles. Bacteria can trigger inflammation and infection resulting in more severe acne.
Four main factors cause acne:
- Excess oil (sebum) production
- Hair follicles clogged by oil and dead skin cells
- Bacteria
- Inflammation
Acne typically appears on your face, forehead, chest, upper back and shoulders because these areas of skin have the most oil (sebaceous) glands. Hair follicles are connected to oil glands.
The follicle wall may bulge and produce a whitehead. Or the plug may be open to the surface and darken, causing a blackhead. A blackhead may look like dirt stuck in pores. But actually the pore is congested with bacteria and oil, which turns brown when it's exposed to the air.
Pimples are raised red spots with a white center that develop when blocked hair follicles become inflamed or infected with bacteria. Blockages and inflammation deep inside hair follicles produce cystlike lumps beneath the surface of your skin. Other pores in your skin, which are the openings of the sweat glands, aren't usually involved in acne.
Certain things may trigger or worsen acne:
- Hormonal changes. Androgens are hormones that increase in boys and girls during puberty and cause the sebaceous glands to enlarge and make more sebum. Hormone changes during midlife, particularly in women, can lead to breakouts too.
- Certain medications. Examples include drugs containing corticosteroids, testosterone or lithium.
- Diet. Studies indicate that consuming certain foods — including carbohydrate-rich foods, such as bread, bagels and chips — may worsen acne. Further study is needed to examine whether people with acne would benefit from following specific dietary restrictions.
- Stress. Stress doesn't cause acne, but if you have acne already, stress may make it worse.
Acne myths
These factors have little effect on acne:
- Chocolate and greasy foods. Eating chocolate or greasy food has little to no effect on acne.
- Hygiene. Acne isn't caused by dirty skin. In fact, scrubbing the skin too hard or cleansing with harsh soaps or chemicals irritates the skin and can make acne worse.
- Cosmetics. Cosmetics don't necessarily worsen acne, especially if you use oil-free makeup that doesn't clog pores (noncomedogenics) and remove makeup regularly. Nonoily cosmetics don't interfere with the effectiveness of acne drugs.
Complications
People with darker skin types are more likely than are people with lighter skin to experience these acne complications:
- Scars. Pitted skin (acne scars) and thick scars (keloids) can remain long-term after acne has healed.
- Skin changes. After acne has cleared, the affected skin may be darker (hyperpigmented) or lighter (hypopigmented) than before the condition occurred.
Risk factors
Risk factors for acne include:
- Age. People of all ages can get acne, but it's most common in teenagers.
- Hormonal changes. Such changes are common during puberty or pregnancy.
- Family history. Genetics plays a role in acne. If both of your parents had acne, you're likely to develop it too.
- Greasy or oily substances. You may develop acne where your skin comes into contact with oil or oily lotions and creams.
- Friction or pressure on your skin. This can be caused by items such as telephones, cellphones, helmets, tight collars and backpacks.